The Barker Hypothesis and the Expanding Scope of Maternal CVD
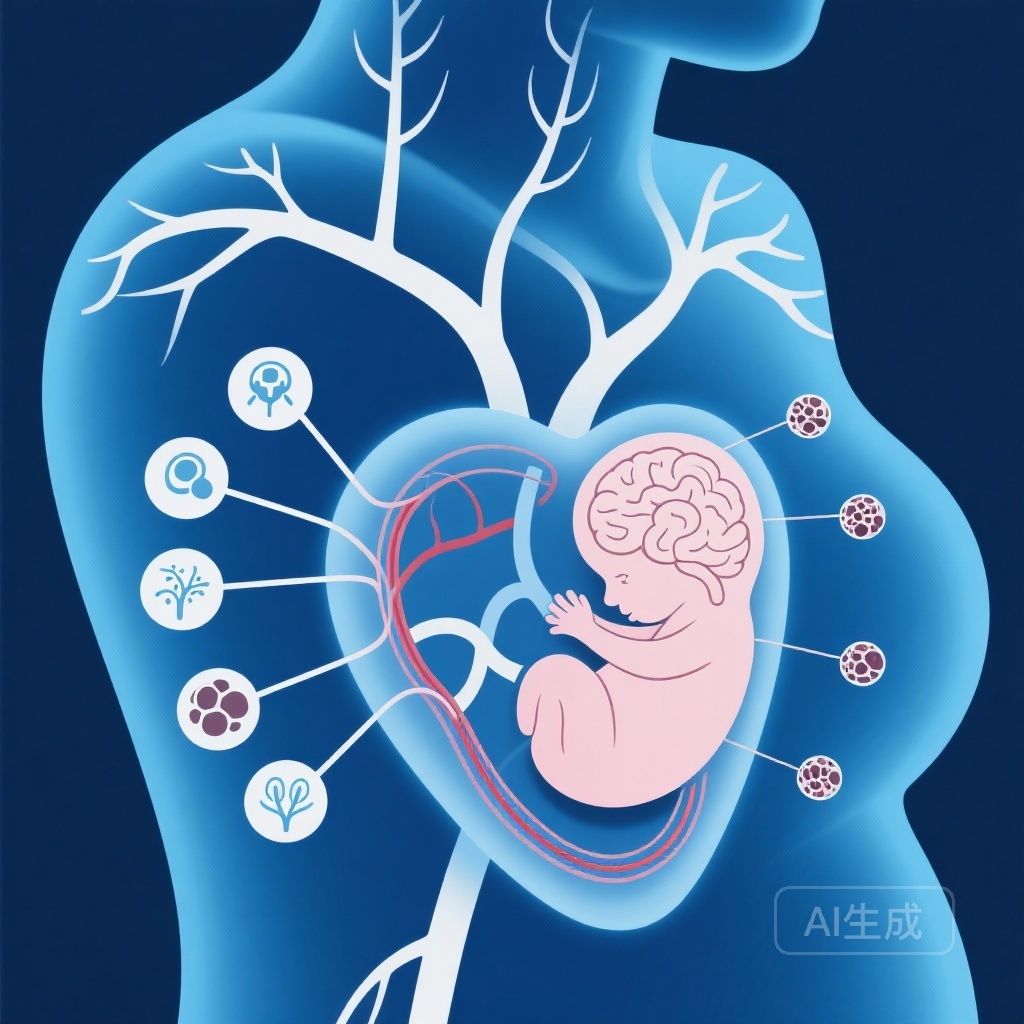
The developmental origins of health and disease (DOHaD) hypothesis, often referred to as the Barker Hypothesis, has long suggested that the intrauterine environment plays a critical role in determining the long-term health trajectory of the offspring. While much research has focused on the impact of gestational diabetes and preeclampsia, the role of maternal pre-existing atherosclerotic cardiovascular disease (ASCVD) has remained relatively underexplored. As the age of first-time mothers increases globally, the prevalence of pre-conception cardiovascular risk factors and established ASCVD is rising, making it a critical area for clinical investigation.
A recent nationwide mother-child paired cohort study published in Human Reproduction Open (Kang et al., 2025) provides significant insights into this association. The study sought to determine whether maternal pre-existing ASCVD—defined by diagnostic codes for myocardial infarction, ischemic stroke, or angina prior to conception—influences both immediate neonatal outcomes and long-term neurodevelopmental trajectories in children.
Study Design and Population Characteristics
To address this question, researchers conducted a massive nationwide cohort study utilizing data from the Korean National Health Insurance Service (KNHIS). The study spanned from 2005 to 2019, linking maternal health records with child health data. The total cohort included 5,461,222 live births from 3,640,815 unique mothers.
Within this population, 145,315 (2.7%) births were to women who had been diagnosed with ASCVD before their pregnancy. To ensure a robust comparison and account for potential confounders, the researchers employed propensity score matching at a 1:4 ratio, adjusting for baseline maternal characteristics such as age, socioeconomic status, and pre-existing comorbidities. Offspring were followed through 2020, allowing for a longitudinal assessment of neurodevelopmental outcomes.
Neonatal Outcomes: Immediate Risks Following Maternal ASCVD Exposure
The study found that offspring born to mothers with pre-existing ASCVD faced significantly higher risks during the neonatal period. The data showed a consistent increase in several adverse outcomes:
- Congenital Malformations: Offspring of mothers with ASCVD had a higher risk of malformations, with an adjusted odds ratio (aOR) of 1.09 (95% CI: 1.07–1.12).
- Neonatal Intensive Care Unit (NICU) Admission: There was a notably higher frequency of NICU admissions among these infants (aOR 1.19, 95% CI: 1.16–1.22).
- Neonatal Sepsis: The risk of developing neonatal sepsis was also elevated, with an aOR of 1.11 (95% CI: 1.07–1.15).
These findings suggest that maternal cardiovascular health impacts the immediate survival and health stability of the neonate, possibly through mechanisms related to placental perfusion or systemic inflammation present even before the onset of pregnancy.
Long-term Trajectory: The Impact on Childhood Neurodevelopment
Perhaps the most striking findings of the study concern the long-term neurodevelopmental health of the children. The researchers tracked the incidence of developmental delay, seizures, and attention-deficit hyperactivity disorder (ADHD) throughout early childhood. The results indicated that maternal ASCVD is a significant risk factor for these conditions, with an adjusted hazard ratio (aHR) of 1.08 (95% CI: 1.07–1.10).
This increased risk remained consistent across different types of neurodevelopmental disorders, suggesting a broad impact on the developing central nervous system. The persistence of these associations through early childhood underscores the potential for maternal cardiovascular pathology to induce long-lasting epigenetic or structural changes in the fetus.
Mechanistic Insights: Exploring the Independent Association
One of the most clinically relevant aspects of this study is the observation that these risks persisted regardless of the presence of adverse pregnancy outcomes (APOs) such as preeclampsia or gestational hypertension. Traditionally, clinicians have viewed the risks to the offspring of women with heart disease as being mediated through these acute pregnancy complications.
However, the findings by Kang et al. suggest an independent contribution of maternal ASCVD. This implies that the underlying pathophysiology of atherosclerosis—including chronic low-grade inflammation, endothelial dysfunction, and impaired microvascular autoregulation—may directly influence fetal development throughout gestation, rather than only through the intermediary of acute placental crises.
Clinical Implications: Refining Preconception and Postnatal Care
The findings of this nationwide cohort study have several implications for clinical practice:
1. Enhanced Preconception Counseling
Women of reproductive age with a history of myocardial infarction, stroke, or angina should be counseled regarding the potential risks to their offspring. This is not to discourage pregnancy but to ensure that cardiovascular health is optimized before conception.
2. Specialized Prenatal Monitoring
Pregnancies in women with pre-existing ASCVD should be categorized as high-risk, requiring multidisciplinary care involving cardiologists, maternal-fetal medicine specialists, and neonatologists. Increased surveillance for fetal growth and placental health is warranted.
3. Early Neurodevelopmental Surveillance
Children born to mothers with ASCVD may benefit from early neurodevelopmental screening. Identifying developmental delays or ADHD early in childhood can lead to more effective interventions and better long-term educational and social outcomes.
Limitations and Considerations
As with any observational study, there are limitations to consider. While propensity score matching was used, residual confounding from factors not captured in the KNHIS database (such as specific dietary habits or detailed smoking history) cannot be entirely excluded. Additionally, the study focused only on live births, which may introduce a survivor bias, as it does not account for the impact of maternal ASCVD on pregnancy loss or stillbirth.
Conclusion
Maternal pre-existing atherosclerotic cardiovascular disease is more than just a maternal health concern; it is a significant determinant of offspring health. By demonstrating a clear link between maternal ASCVD and both neonatal complications and long-term neurodevelopmental disorders, this study highlights a critical window for intervention. Clinicians must prioritize cardiovascular health in women of reproductive age and maintain a high index of suspicion for developmental challenges in their children.
Funding and Trial Registration
This study was supported by the Patient-Centered Clinical Research Coordinating Center (PACEN) funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HC21C0123) and the Bio&Medical Technology Development Program of the National Research Foundation (NRF) funded by the Korean government (MSIT) (No. RS-2024-00440881). The study is registered at ClinicalTrials.gov (NCT06406998).
References
Kang D, Heo J, Choi KH, Park T, Sung JH, Park TK, Lee JM, Cho J, Yang JH, Song YB, Hahn JY, Choi SH, Gwon HC, Oh SY. Association of maternal pre-existing atherosclerotic cardiovascular disease and neonatal and long-term offspring outcomes: a nationwide mother-child paired cohort. Hum Reprod Open. 2025 Nov 25;2025(4):hoaf074. doi: 10.1093/hropen/hoaf074. PMID: 41383953.