Highlights
– In a randomized noninferiority trial (N=156), manual marking-assisted capsulorhexis (MMAC) was noninferior to digital-guidance–assisted capsulorhexis (DGAC) for capsulorhexis diameter accuracy after phacoemulsification.
– Median deviations from the target diameter were small in both groups (horizontal: 0.22 mm MMAC vs 0.27 mm DGAC; vertical: 0.27 mm vs 0.33 mm) and within the pre-specified noninferiority margin of 0.20 mm.
– The proportion of ‘‘ideal’’ capsulorhexis was high in both arms (96.2% MMAC vs 88.5% DGAC), suggesting clinical equivalence in well-selected patients with adequately dilated pupils.
Background
Successful phacoemulsification cataract surgery depends on a well-centered, appropriately sized continuous curvilinear capsulorhexis (CCC). CCC size and centration determine anterior capsule overlap on the intraocular lens (IOL), influence effective lens position, and affect long-term IOL centration and stability—issues that are especially important for premium IOLs (toric, multifocal, extended depth of focus) where centration and tilt materially affect visual outcomes.
Digital guidance systems (image-guided overlays or intraoperative projection rings) and femtosecond laser capsulotomy have been developed to improve reproducibility of capsulorhexis. However, such technologies are not universally available because of cost and infrastructure requirements. A pragmatic, low-cost, device-free manual marking method that reliably guides CCC could expand access and standardize results across diverse practice settings.
Study design
Chen et al. conducted a single-center, randomized, noninferiority clinical trial at Zhongshan Ophthalmic Center, China (July–December 2021) with 1-month follow-up. The trial enrolled adults aged 55–80 years with age-related cataract, pupil diameter ≥6.5 mm after dilation, and Lens Opacities Classification System III nuclear opalescence grade 3.0–4.0. Exclusion criteria included prior intraocular surgery or ocular conditions likely to affect zonular integrity.
Participants (n=156) were randomized 1:1 to:
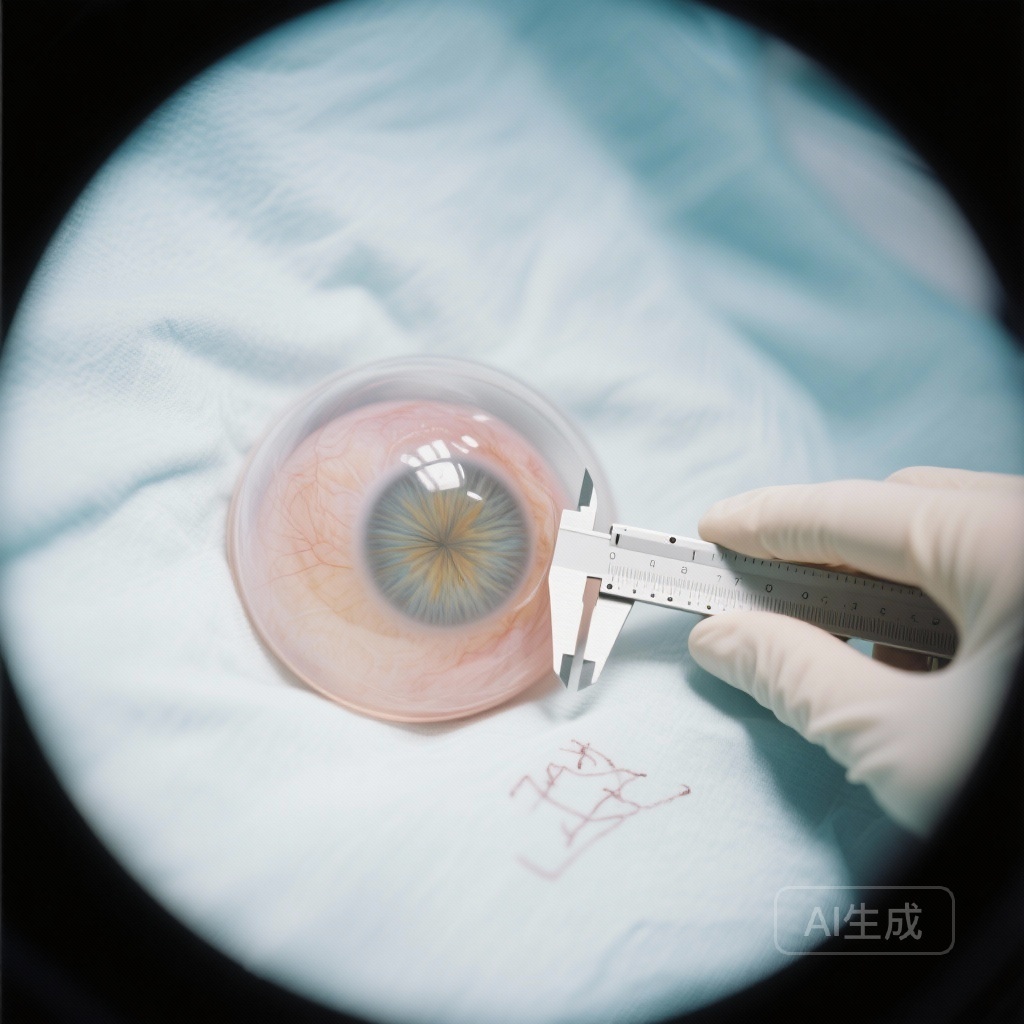
- MMAC: surgeon used a lens caliper to measure and locate the intended capsulorhexis center and applied the blunt caliper head to the anterior lens capsule to create a temporary mark visible intraoperatively for CCC guidance.
- DGAC: a pre-defined ring of target diameter was projected (digital guidance) to guide CCC.
The primary outcome was the median deviation of the achieved capsulorhexis diameter from the target diameter (horizontal and vertical), with a pre-specified noninferiority margin of 0.20 mm. Secondary outcomes included proportion of ‘‘ideal’’ capsulorhexis (clinically defined), grades of capsulorhexis–IOL overlap, off-center distance of capsulorhexis, postoperative best-corrected visual acuity (BCVA), and IOL tilt and decentration. Data were analyzed September–December 2024. Trial registration: ClinicalTrials.gov NCT04977115.
Key findings
Population: Of 204 adults screened, 156 met inclusion criteria and were randomized equally (n=78 per arm). Mean age was 71–72 years in both groups; each arm comprised 60% female participants.
Primary outcome — capsulorhexis diameter accuracy
Median deviation between the performed capsulorhexis and the target diameter (horizontal) was 0.22 mm (95% CI, 0.11–0.37) in the MMAC group versus 0.27 mm (95% CI, 0.14–0.52) in the DGAC group. The between-group difference was −0.05 mm (95% CI, −0.16 to 0.07). For the vertical diameter the median deviations were 0.27 mm (95% CI, 0.12–0.40) for MMAC and 0.33 mm (95% CI, 0.20–0.51) for DGAC (difference −0.06 mm; 95% CI, −0.17 to 0.05). In both dimensions the 95% confidence intervals of the differences lay within the pre-specified noninferiority margin of 0.20 mm, satisfying the noninferiority hypothesis.
Secondary outcomes
The proportion of ‘‘ideal’’ capsulorhexis was 96.2% (75 of 78) in the MMAC arm and 88.5% (69 of 78) in the DGAC arm (difference 7.7%; 95% CI, −0.6 to 16.0), also meeting the study’s noninferiority criterion of −5.0%. Measures of capsulorhexis–IOL overlap, off-center distance, postoperative BCVA, IOL tilt, and decentration showed no clinically meaningful differences between groups at 1 month, consistent with equivalent short-term optical outcomes in this selected cohort.
Safety and intraoperative considerations
No unexpected safety signals were reported. The trial population excluded eyes with small pupils, complex cataracts, or zonular compromise, so findings reflect outcomes achievable in routine, uncomplicated cases with adequate dilatation and experienced surgical technique.
Expert commentary
Strengths of the trial include randomized allocation, a pragmatic and clinically relevant noninferiority design, and clearly defined primary and secondary outcomes focused on capsulorhexis metrics that matter for IOL behavior. The use of a simple, reproducible manual marking technique that requires only an inexpensive lens caliper addresses an important accessibility gap where digital systems are unavailable.
Limitations to consider:
- Single-center setting and enrollment of only patients with pupils ≥6.5 mm and relatively dense but uncomplicated cataracts limit generalizability to small-pupil, shallow anterior chamber, white cataract, or zonular weakness cases where visualization and capsulorhexis control are more challenging.
- Surgeon experience was not described in full detail in this summary; outcomes may depend on operator skill with the manual marking method.
- Follow-up was limited to 1 month. Longer-term implications for IOL position, posterior capsular opacification, and refractive predictability were not assessed here and are important for premium IOLs where subtle centration differences can manifest clinically over time.
- While the study demonstrates equivalence in diameter and short-term centration metrics, it does not substitute for femtosecond laser capsulotomy studies that evaluate capsule strength, geometry, and potential downstream effects in other contexts.
Clinical implications: For routine adult cataract surgery with adequate pupil dilation and cooperative anatomy, MMAC offers a low-cost, scalable strategy to achieve precise capsulorhexis sizing and centration comparable to a digital guidance system. This can be particularly valuable in low-resource settings or high-volume practices where access to image-guided overlays or femtosecond platforms is limited.
Biological plausibility and mechanistic notes
CCC reproducibility depends on identifying a stable ocular reference (limbus, pupil, or capsular landmarks) and translating that reference to the anterior capsule. The MMAC approach effectively creates a localized visual cue on the capsule itself, reducing reliance on external projection accuracy and potential eye–device registration errors. In eyes with stable anatomy and clear visualization, a direct mark on the capsule provides a robust intraoperative guide for manual tearing of the capsule along a planned curve.
Conclusion
This randomized noninferiority trial supports that a simple, device-free manual marking-assisted capsulorhexis (MMAC) achieves capsulorhexis diameter accuracy and short-term centration comparable to a digital guidance-assisted technique in carefully selected patients undergoing phacoemulsification. MMAC may be a practical alternative in settings lacking digital guidance systems, but wider adoption should consider surgeon training, case selection, and the need for longer-term outcome data, especially when implanting premium IOLs.
Clinical practice implications and research gaps
Practically, MMAC can be taught and implemented with minimal cost. Training curricula could include standardized steps for caliper-based measurement and marking, and quality assurance might track achieved capsulorhexis diameters and IOL overlap for ongoing audit. Future research should address: (1) performance in challenging anatomy (small pupils, shallow chambers, zonular laxity), (2) reproducibility across surgeons with variable experience, (3) long-term IOL stability and refractive outcomes, and (4) specific performance with premium IOLs where submillimeter differences may be clinically relevant.
Funding and clinicaltrials.gov
Trial registration: ClinicalTrials.gov Identifier: NCT04977115. Funding details and disclosures are reported in the original publication by Chen et al.; readers should consult the full paper for declarations of funding and conflicts of interest.
References
1. Chen X, Liu Z, Jin L, Zheng Y, Luo L, Liu Y. Manual Marking Guidance vs Digital Guidance System-Assisted Capsulorhexis in Phacoemulsification: A Noninferiority Randomized Clinical Trial. JAMA Ophthalmol. 2025 Nov 13. doi: 10.1001/jamaophthalmol.2025.4448. Epub ahead of print. PMID: 41231447.
2. American Academy of Ophthalmology Cataract Preferred Practice Pattern Panel. Cataract in the Adult Eye: Preferred Practice Pattern. American Academy of Ophthalmology; latest edition online. (Consult original for updates and full recommendations.)
Note: This article is a critical interpretation of the trial by Chen et al. and does not substitute for reading the original paper for complete methods, full results, and disclosures.