Highlights
- The LASSO trial found no statistically significant difference in 5-year recurrence rates of small bowel obstruction (SBO) between laparoscopic and open adhesiolysis (12.5% vs. 9.7%).
- Incisional hernia incidence was nearly identical between the two groups (6.3% for laparoscopy vs. 6.1% for open surgery).
- Patient-reported quality of life, measured by SF-36 and GIQLI, showed no significant long-term divergence after 5 years.
- While laparoscopy remains a viable option for selected patients due to faster initial recovery, it does not appear to alter the long-term natural history of adhesive bowel disease.
Background: The Evolution of SBO Management
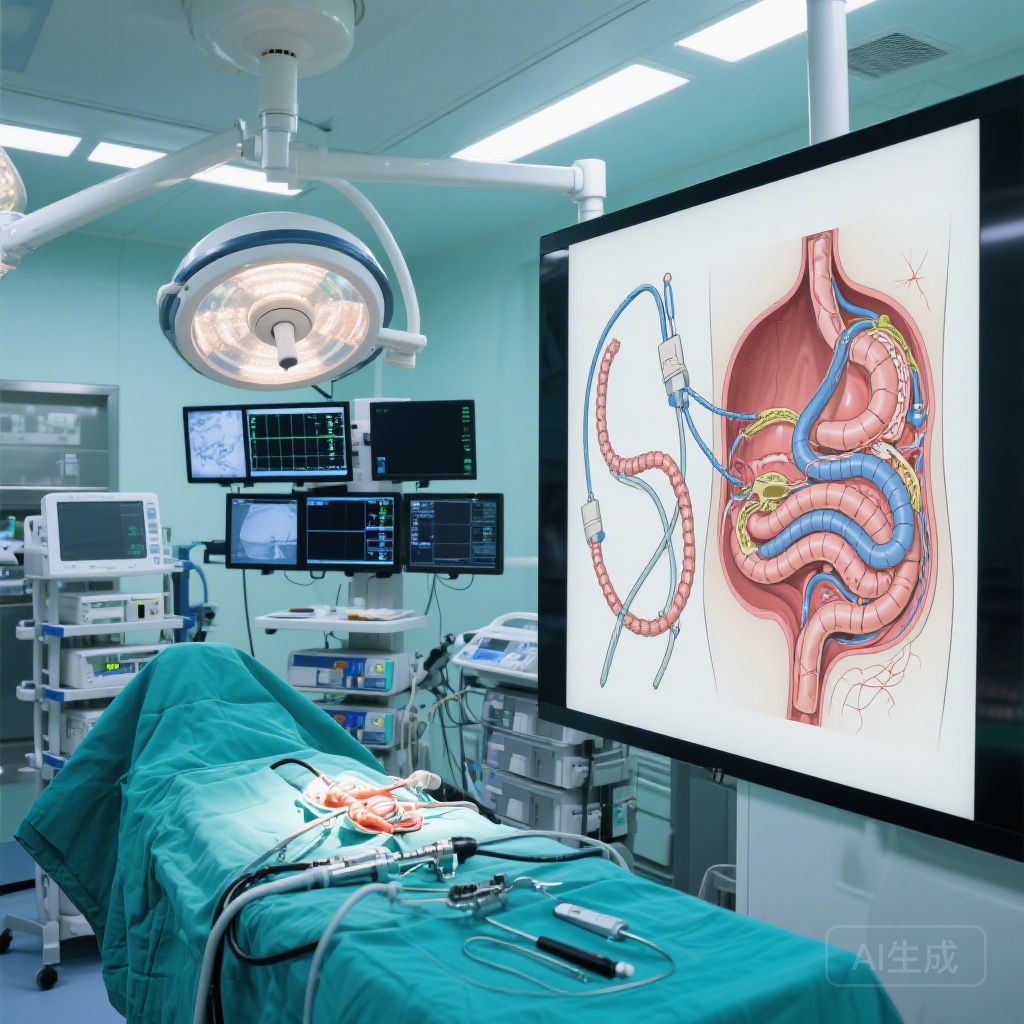
Adhesive small bowel obstruction (SBO) remains a leading cause of emergency surgical admissions worldwide, imposing a significant burden on healthcare systems and patient quality of life. Traditionally, the management of SBO that failed conservative measures was the domain of open surgery (laparotomy). However, the rise of minimally invasive surgery has led to the increasing adoption of laparoscopic adhesiolysis.
Proponents of the laparoscopic approach point to well-documented short-term benefits, including reduced postoperative pain, shorter hospital stays, and quicker return to bowel function. Yet, a critical question has persisted: does the surgical approach influence the long-term risk of recurrence or the development of late complications like incisional hernias? Given that adhesions themselves are often the result of prior surgical trauma, the hypothesis that a less invasive approach might lead to fewer future adhesions and complications is theoretically sound but required rigorous clinical validation.
Study Design: The LASSO Randomized Clinical Trial
The Laparoscopic vs Open Adhesiolysis for Adhesive Small Bowel Obstruction (LASSO) trial was designed to provide high-level evidence addressing this gap. Conducted across eight hospitals in Finland and Italy between July 2013 and April 2018, the trial initially focused on short-term recovery. This latest report provides the crucial 5-year follow-up data, analyzing long-term outcomes in a parallel, open-label randomized framework.
Participants and Methodology
The study included 104 randomized patients presenting with clinical and radiological signs of adhesive SBO that did not resolve with conservative management. Following exclusions and dropouts, 100 patients (mean age 69.2 years; 65% female) were included in the final analysis: 49 in the open surgery group and 51 in the laparoscopic group. The data were analyzed using modified intention-to-treat and post hoc per-protocol analyses to ensure robust conclusions.
Primary and Secondary Endpoints
The long-term analysis focused on three primary domains:
1. SBO recurrence rates (both clinical and those requiring surgery).
2. Incisional hernia incidence.
3. Long-term Quality of Life (QOL), assessed via the Gastrointestinal Quality of Life Index (GIQLI) and the 36-item Short-Form Health Survey (SF-36).
Key Findings: Long-Term Outcomes at 5 Years
The results of the LASSO trial suggest that the initial surgical approach—whether laparoscopic or open—does not significantly dictate the five-year clinical trajectory of patients with adhesive SBO.
SBO Recurrence
At the 1-year mark, recurrence was rare in both groups: 2.3% in the open group vs. 4.5% in the laparoscopy group. By the 5-year follow-up, the cumulative recurrence rate increased but remained comparable between groups. Specifically, 9.7% (3 patients) in the open-surgery group experienced at least one recurrence, compared to 12.5% (4 patients) in the laparoscopy group. The odds ratio (OR) was 1.33 (95% CI, 0.27-6.51), with a p-value > .99, indicating no statistical difference.
Incisional Hernia Incidence
One of the theoretical advantages of laparoscopy is the reduction of large abdominal incisions, which should, in theory, lower the risk of incisional hernias. However, the LASSO data did not support this advantage in long-term follow-up. Incisional hernias were detected in 6.1% of the open group and 6.3% of the laparoscopy group (OR, 1.03; 95% CI, 0.14-7.82; p > .99). This suggests that the risk of hernia may be driven more by patient-specific factors or the necessity of the umbilical/port-site incisions rather than the length of the primary laparotomy incision alone.
Quality of Life Metrics
Patient-reported outcomes are increasingly recognized as essential measures of surgical success. At 5 years, the median SF-36 score was 73.2 in the open group vs. 67.1 in the laparoscopy group (p = .23). Similarly, GIQLI scores were nearly identical, with a median of 118 for open surgery and 119 for laparoscopy (p = .54). These results indicate that the initial surgical technique does not have a lasting impact on a patient’s subjective health status or gastrointestinal function half a decade later.
Expert Commentary: Interpreting the Data
The findings of the LASSO trial provide a sobering reality check for the surgical community. While the laparoscopic approach is undeniably superior in the immediate postoperative phase—offering faster discharge and less acute pain—these benefits appear to be transient. The lack of superiority in long-term outcomes suggests that the underlying pathophysiology of adhesion formation and the patient’s predisposition to hernias are not significantly mitigated by the choice of surgical access.
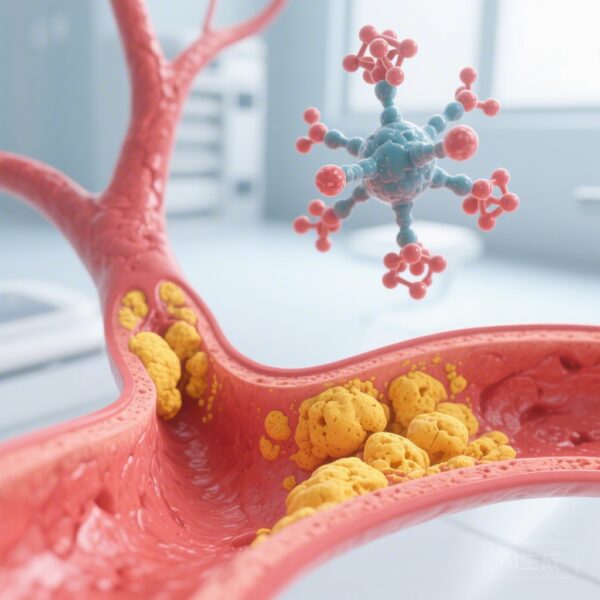
Mechanistic Insights
One possible explanation for the lack of difference in recurrence is that while laparoscopy involves smaller incisions, the intra-abdominal trauma required to mobilize the bowel and lyse adhesions remains substantial. The biological triggers for fibrin deposition and subsequent adhesion formation occur regardless of the size of the abdominal wall incision. Furthermore, the conversion rate from laparoscopy to open surgery (often cited in other literature) can dilute the benefits of the minimally invasive approach, although this trial utilized intention-to-treat analysis to account for such real-world complexities.
Clinical Implications
For clinicians, these results reinforce that the decision to use laparoscopy should be based on patient selection, surgeon expertise, and the goal of achieving rapid short-term recovery. It should not be marketed to patients as a way to “prevent” future obstructions or hernias compared to open surgery. In cases where laparoscopy is technically demanding or potentially unsafe due to extreme distention or dense adhesions, the surgeon should feel confident that reverting to or starting with an open approach does not disadvantage the patient in the long run.
Conclusion: A Balanced Perspective
The LASSO randomized clinical trial confirms that laparoscopic adhesiolysis is a safe and effective alternative to open surgery for SBO, but it is not a panacea for the long-term complications of adhesive disease. At 5 years, there were no significant differences in recurrence, hernia rates, or quality of life. Surgeons should continue to offer the laparoscopic approach to suitable candidates to capitalize on short-term recovery benefits, while maintaining realistic expectations regarding the long-term natural history of the condition.
Funding and Trial Information
The LASSO trial was conducted as an international multicenter study. Trial registration: ClinicalTrials.gov Identifier: NCT01867528. Analysis was conducted from February to May 2025.
References
1. Räty P, Mentula P, Haukijärvi E, et al. Long-Term Outcomes After Laparoscopic vs Open Adhesiolysis for Small Bowel Obstruction: The LASSO Randomized Clinical Trial. JAMA Surg. 2026 Feb 18. doi: 10.1001/jamasurg.2025.6726.
2. Ten Broek RPG, Issa Y, van Santbrink EJP, et al. Burden of adhesions in abdominal and pelvic surgery: systematic review and met-analysis. BMJ. 2013;347:f5588.
3. Sallinen V, Di Saverio S, Haukijärvi E, et al. Laparoscopic versus open adhesiolysis for adhesive small bowel obstruction (LASSO): an international, multicentre, randomised, open-label trial. Lancet Gastroenterol Hepatol. 2019;4(4):278-286.