Introduction
The management of frozen-thawed embryo transfer (FET) has undergone a significant paradigm shift over the last decade. Clinicians are increasingly moving away from medicated cycles (hormone replacement therapy, or HRT) toward protocols that preserve the corpus luteum (CL). The absence of a CL in HRT-FET has been linked to an increased risk of hypertensive disorders of pregnancy and other obstetric complications. However, natural cycles (NC) present logistical challenges regarding clinical scheduling and timing the window of implantation (WOI).
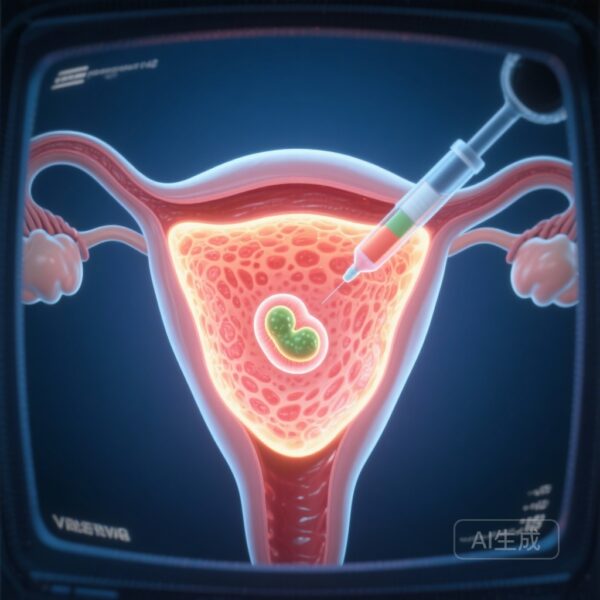
A recent multi-centric prospective cohort study by Eggersmann et al. (2025) explores a middle ground: the ‘Programmed-Ovulatory FET’ (PO-FET) protocol. This approach uses oral dydrogesterone (DYD) initiated in the late follicular phase to schedule the timing of the embryo transfer while allowing for endogenous ovulation and CL formation. Critically, the study investigates whether the serum levels of these steroids on the day of transfer actually influence the ultimate clinical goal: a live birth.
Highlights
1. High Ovulation Success
The PO-FET protocol, utilizing 30 mg oral dydrogesterone daily, was compatible with endogenous ovulation in 98.1% of cases, as evidenced by serum progesterone levels exceeding 1.5 ng/ml on the day of embryo transfer.
2. No Hormone Threshold for Success
Serum levels of dydrogesterone (DYD), its primary metabolite 20α-dihydrodydrogesterone (DHD), progesterone (P), and estradiol (E2) on the day of FET showed no consistent relationship with live birth rates, whether analyzed individually or in interaction.
3. Simplified Monitoring
The findings suggest that in ovulatory cycles supplemented with dydrogesterone, the intensive monitoring of serum sex-steroid levels on the transfer day may be clinically unnecessary, simplifying the patient journey and reducing healthcare costs.
Background: The Evolution of Luteal Phase Support
Standard HRT regimens for FET rely entirely on exogenous estrogen and progesterone. While effective for scheduling, these regimens are under scrutiny for two main reasons. First, there is a risk of insufficient progesterone exposure due to individual variations in absorption or vaginal administration issues. Second, the iatrogenic absence of the corpus luteum deprives the maternal-fetal interface of essential vasoactive factors like relaxin and prorenin, which are thought to be protective against pre-eclampsia.
Dydrogesterone, a retroprogesterone with high oral bioavailability and specificity for the progesterone receptor, has emerged as a potent alternative. Unlike micronized progesterone, DYD does not cross-react with standard progesterone immunoassays, allowing clinicians to measure endogenous progesterone production (from the CL) even while the patient is taking exogenous support. The ‘Programmed-Ovulatory’ approach leverages this to create a predictable transfer schedule while maintaining the physiological benefits of an ovulatory cycle.
Study Design and Methodology
This research was nested within a larger multi-centric, prospective clinical cohort study (NCT03507673). The analysis included 559 normally cycling women undergoing FET in a spontaneous menstrual cycle between December 2021 and August 2023.
Patient Monitoring and Protocol
Beginning on cycle day 10, participants underwent serial endocrine (E2, LH, P) and sonographic monitoring. The criteria for initiating the PO-FET protocol included a leading follicle of ≥16 mm, an endometrial thickness of ≥6 mm, and E2 levels of ≥180 pg/ml. Once these criteria were met, oral DYD (10 mg, three times daily) was initiated. If no LH surge was detected, the initiation could be adjusted within a two-day window to suit clinical or patient preferences, effectively ‘programming’ the transfer. Embryo transfer occurred on the 3rd to 6th day of DYD intake, depending on the embryo’s developmental stage (Day 2 to Day 5).
Analytical Techniques
A key strength of this study was the use of high-performance liquid chromatography/tandem mass spectroscopy (HPLC/MS/MS) and electrochemiluminescence immunoassay (ECLIA) to precisely measure serum levels of DYD and its active metabolite DHD, alongside P and E2.
Key Findings: Does the Hormone Level Matter?
The primary objective was to determine if hormone levels on the day of FET influenced live birth rates. The results were largely negative, which in this context, provides a liberating conclusion for clinical practice.
Ovulatory Rates and Progesterone Levels
The study confirmed that late follicular phase initiation of DYD does not suppress ovulation. Serum progesterone levels indicated successful ovulation (>1.5 ng/ml) in 98.1% of FETs involving Day 4 or 5 embryos. Furthermore, 95.4% of these cases reached a P level >3.0 ng/ml. Interestingly, progesterone levels were significantly higher in cycles involving Day 4/5 embryos compared to Day 2/3 embryos, likely reflecting the further progression of the luteal phase.
Hormone Levels vs. Live Birth Rates
The researchers stratified patients into low (≤25th percentile) and normal-high (>25th percentile) hormone levels. They found no statistically significant differences in live birth risk differences (RD) for any of the measured steroids:
- DYD: RD -5.3% (P = 0.227)
- DHD: RD -4.0% (P = 0.428)
- Progesterone: RD 2.9% (P = 0.597)
- Estradiol: RD -3.3% (P = 0.487)
Logistic regression across the entire range of hormone values confirmed these findings. There were no ‘threshold’ levels identified below which pregnancy success significantly dropped, nor were there interaction effects between the hormones (e.g., high DYD compensating for low P).
Expert Commentary and Clinical Interpretation
The lack of correlation between dydrogesterone levels and clinical outcomes is particularly noteworthy. In HRT cycles, recent literature has suggested a minimum threshold for serum progesterone (often cited around 9–11 ng/ml) to optimize pregnancy rates. However, in the PO-FET protocol, the presence of the corpus luteum appears to provide a ‘safety net’.
Biological Plausibility
Because the corpus luteum produces progesterone directly into the local circulation and maintains its own regulatory feedback loops, the exact systemic concentration of exogenous dydrogesterone may be less critical than in a cycle where the CL is absent. Furthermore, DYD’s high affinity for the progesterone receptor means that even low systemic concentrations may be sufficient for endometrial transformation when combined with endogenous production.
Limitations to Consider
The authors acknowledge that this was not an intention-to-treat analysis; outcomes were only assessed for those who actually proceeded to FET. Additionally, while the protocol is ‘ovulatory,’ the administration of progestins in the late follicular phase can still interfere with the natural LH surge and luteal characteristics. Future randomized controlled trials (RCTs) are needed to compare PO-FET directly against ‘True’ Natural Cycle FET and Managed NC-FET (hCG trigger).
Conclusion
The ‘Programmed-Ovulatory FET’ protocol represents a significant refinement in assisted reproductive technology. It offers the scheduling convenience of an HRT cycle with the physiological and safety advantages of a natural cycle. The finding that live birth rates are unrelated to sex-steroid levels on the day of FET suggests that clinicians can move away from the ‘anxiety of the threshold’—the constant monitoring and adjustment of progesterone doses—provided that ovulation is confirmed. This injection-free, low-cost, and patient-friendly protocol is a robust candidate for the new standard of care in frozen embryo transfer.
Funding and Registration
The trial was supported by institutional resources of the University Hospital of Schleswig-Holstein, Campus Lübeck. ClinicalTrials.gov Identifier: NCT03507673.
References
1. Eggersmann TK, et al. Live birth rates are unrelated to sex-steroid levels on ET day in a dydrogesterone-based ‘programmed-ovulatory FET’ protocol: a multi-centric prospective cohort study. Hum Reprod Open. 2025;2025(4):hoaf058.
2. Griesinger G, et al. Oral dydrogesterone versus intravaginal micronized progesterone for luteal phase support in IVF: a systematic review and meta-analysis. Fertil Steril. 2018;109(6):1016-1027.
3. von Wolff M, et al. The corpus luteum: a forgotten organ in modern assisted reproduction? Hum Reprod Update. 2021;27(3):412-427.