Introduction: The Persistent Challenge of Brain Metastases
Brain metastases (BMs) represent one of the most formidable hurdles in the management of advanced breast cancer (BC). While the advent of HER2-targeted therapies has significantly improved outcomes for patients with HER2-positive disease, those with HER2-negative (HER2-) subtypes—including hormone receptor-positive (HR+) and triple-negative breast cancer (TNBC)—continue to face a dismal prognosis. Once the disease crosses the blood-brain barrier (BBB), systemic treatment options become limited due to poor drug penetration and the unique microenvironment of the central nervous system (CNS).
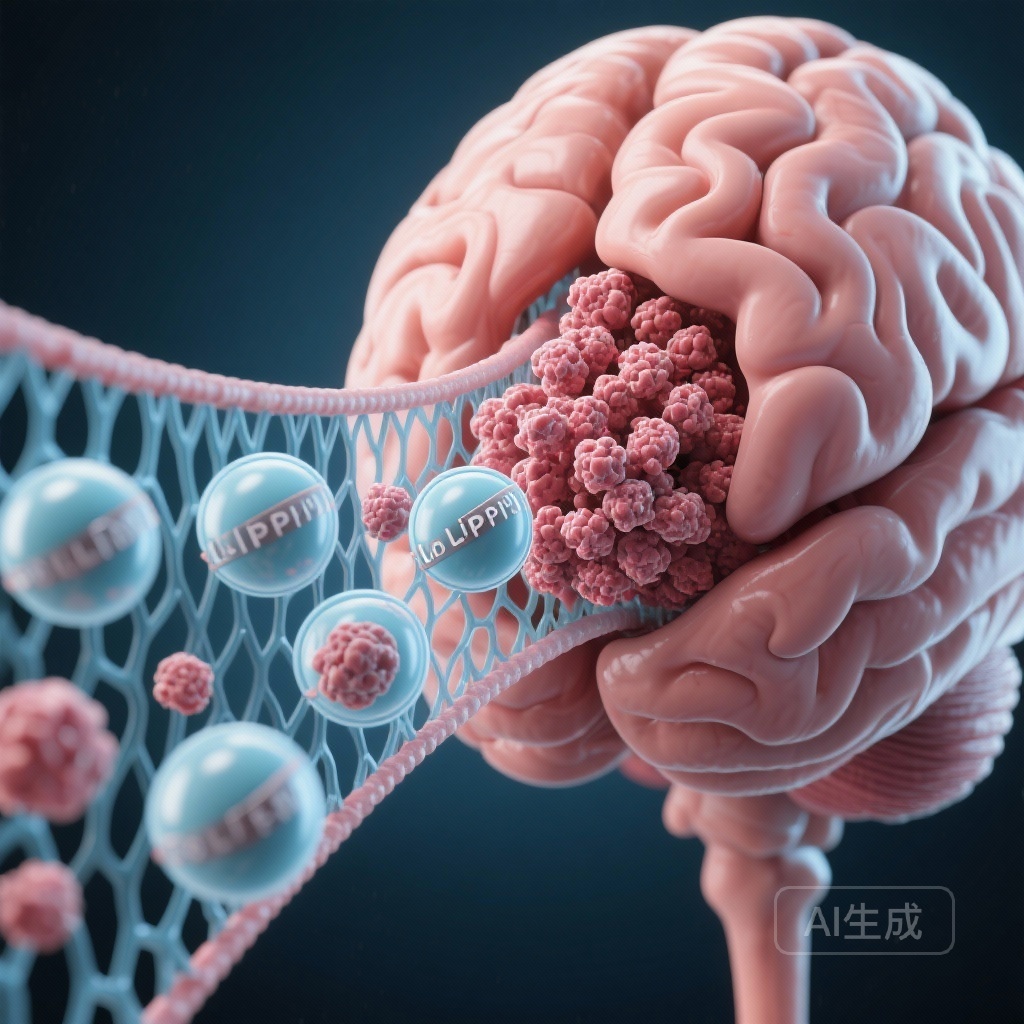
TNBC, in particular, exhibits a high propensity for early CNS involvement, often occurring while systemic disease remains controlled. The standard of care has historically relied on local interventions, such as whole-brain radiation therapy (WBRT), stereotactic radiosurgery (SRS), or surgical resection. However, these modalities do not address the systemic nature of the disease, and their repetitive use is limited by neurotoxicity. Consequently, there is an urgent clinical demand for CNS-active systemic agents. Liposomal irinotecan (nal-IRI), a nanotherapeutic formulation of the topoisomerase I inhibitor irinotecan, has emerged as a candidate of interest due to its ability to leverage the enhanced permeability and retention (EPR) effect to bypass the BBB more effectively than its non-liposomal counterpart.
The PHENOMENAL Study: Rationale and Design
The PHENOMENAL study (NCT03328884) was designed as a single-arm, open-label, multicenter phase 2a trial conducted across 16 sites in Spain. The primary objective was to evaluate the intracranial activity and safety of nal-IRI in patients with HER2-negative breast cancer and brain metastases. The rationale for using a liposomal formulation lies in its pharmacokinetic profile: nal-IRI encapsulates irinotecan in long-circulating liposomes, which protects the active drug from premature metabolism and facilitates its accumulation in tumor tissues where the vasculature is compromised—a phenomenon often seen in the “blood-tumor barrier” of brain metastases.
Patient Population and Eligibility
The study enrolled 56 women with a median age of 52 years. Eligibility criteria included confirmed HER2-negative metastatic breast cancer with active or stable BMs. Crucially, the cohort was heavily pretreated; all patients had received at least one prior taxane-based regimen for metastatic disease. Of the participants, 51.8% had TNBC, and a staggering 91.1% presented with progressive BMs at the time of baseline, making this a particularly high-risk and difficult-to-treat population.
Treatment Protocol
Patients received nal-IRI intravenously at a dose of 60 mg/m2 (salt-base) or 50 mg/m2 (free-base) every 14 days. This dosing schedule continued until disease progression or the occurrence of unacceptable toxicity. The primary endpoint was the intracranial objective response rate (IC-ORR), specifically measured in patients with progressive BMs. Secondary endpoints included systemic objective response rate (ORR), clinical benefit rate (CBR), progression-free survival (PFS), overall survival (OS), and a comprehensive safety analysis.
Key Findings: Intracranial Efficacy and Survival
The PHENOMENAL trial successfully met its primary endpoint, providing statistically significant evidence of intracranial activity. Among patients with progressive BMs, the IC-ORR was 22.0% (95% CI, 11.5–36.0; p < 0.001). This response rate is noteworthy given the heavily pretreated nature of the cohort and the lack of established systemic therapies for these patients.
Survival Outcomes
While the intracranial response was encouraging, the survival data highlighted the aggressive nature of the disease in this setting. The median progression-free survival (PFS) was 1.5 months (95% CI, 1.4–2.9). This relatively short PFS suggests that while nal-IRI can induce rapid tumor shrinkage in the brain, maintaining that response in a late-line setting remains a challenge. The median overall survival (OS) reached 6.4 months (95% CI, 4.9–10.8). Although these numbers appear modest, they must be interpreted within the context of a population where median survival is often measured in weeks once BMs become progressive.
Safety and Tolerability
The safety profile of nal-IRI in this study was consistent with its known effects in other indications, such as pancreatic cancer. Treatment-emergent adverse events (TEAEs) occurred in 96.4% of patients, but only 57.1% were deemed treatment-related. Grade 3 or higher treatment-related events were reported in 14.3% of the cohort. Importantly, serious treatment-related events were rare (occurring in only one patient), and no treatment-related deaths were recorded. Common toxicities included gastrointestinal issues (diarrhea, nausea) and hematological effects (neutropenia), which were generally manageable with standard supportive care and dose adjustments.
Expert Commentary: Mechanistic Insights and Clinical Utility
The success of nal-IRI in achieving a 22% IC-ORR is a testament to the evolution of nanomedicine in oncology. Traditional irinotecan is quickly converted to its active metabolite, SN-38, which has a short half-life and limited CNS penetration. The liposomal carrier essentially acts as a “Trojan horse,” protecting the payload until it reaches the tumor site. Once within the tumor microenvironment, macrophages often take up the liposomes and release the drug, providing a sustained concentration of SN-38 directly at the site of the brain lesion.
However, the discrepancy between the IC-ORR and the short median PFS indicates a need for strategic refinement. Experts suggest that nal-IRI might be more effective if utilized in earlier lines of therapy or in combination with other agents, such as PARP inhibitors or immunotherapy, particularly for the TNBC subgroup. Furthermore, the PHENOMENAL study underscores the importance of the RANO-BM (Response Assessment in Neuro-Oncology Brain Metastases) criteria in clinical trials, as they provide a more accurate reflection of CNS-specific drug activity compared to traditional RECIST criteria.
Limitations and Generalizability
The primary limitation of the study is its single-arm design and relatively small sample size, which prevents direct comparison with other regimens. Additionally, the inclusion of both HR+ and TNBC patients, while reflective of clinical practice, introduces heterogeneity in tumor biology that might influence response patterns. Future studies should consider stratifying results by molecular subtype to determine if one group derives more benefit than the other.
Conclusion: A Stepping Stone for Future Research
The PHENOMENAL study confirms that liposomal irinotecan possesses clinically meaningful intracranial activity in HER2-negative breast cancer patients with brain metastases. While the overall efficacy was limited by the advanced stage of the disease and the short duration of response, the trial provides a critical “proof of concept” for the use of liposomal topoisomerase inhibitors in neuro-oncology.
For clinicians, these results offer a potential systemic option for a patient population that has long been excluded from clinical trials. Moving forward, the focus must shift toward identifying biomarkers of response and exploring combination strategies that can extend the durability of the intracranial responses observed here. The unmet need in HER2-negative brain metastases remains vast, but the PHENOMENAL trial represents a significant step toward filling that void.
Funding and Clinical Trial Information
The PHENOMENAL study (NCT03328884) was supported by various oncology research grants and multicenter collaborations in Spain. For detailed trial information and full data sets, clinicians are encouraged to visit clinicaltrials.gov.
References
1. Borrego MR, López-Bravo DP, Vila MM, et al. Liposomal irinotecan in patients with HER2-negative breast cancer and brain metastases: The PHENOMENAL phase 2 study. Eur J Cancer. 2026;233:116161. doi:10.1016/j.ejca.2025.116161.
2. Lin NU, Bellon JR, Winer EP. CNS metastases in breast cancer. J Clin Oncol. 2004;22(14):2890-2898.
3. Zhang L, et al. The EPR effect and beyond: Strategies to improve tumor targeting of nanomedicines. ACS Nano. 2017;11(10):9569-9576.