Study Background and Disease Burden
Non-alcoholic fatty liver disease (NAFLD), also referred to as metabolic-associated fatty liver disease (MAFLD), constitutes a rapidly escalating global health problem closely linked with obesity, insulin resistance, and metabolic syndrome. Characterized by excessive hepatic fat accumulation in the absence of significant alcohol intake, NAFLD affects approximately 25% of the worldwide population and predisposes individuals to progressive liver inflammation, fibrosis, cirrhosis, and hepatocellular carcinoma. Despite its prevalence and significant morbidity, approved pharmacological treatments remain lacking, underscoring an urgent need for novel, effective therapies.
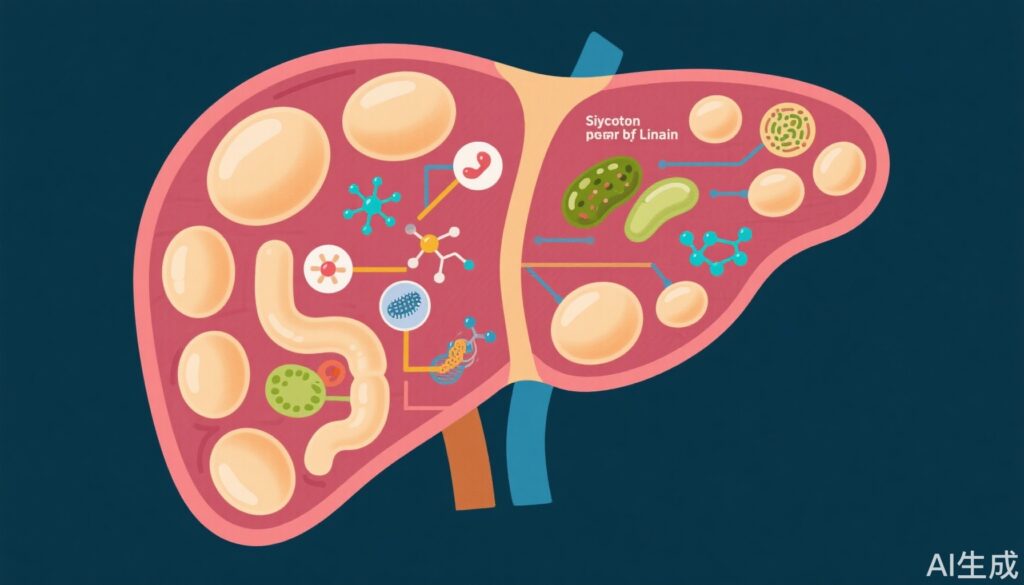
Pathophysiologically, NAFLD is linked to complex mechanisms involving lipid metabolism dysregulation, oxidative stress, inflammation, mitochondrial dysfunction, impaired autophagy, and gut microbiota dysbiosis. Therapeutic strategies targeting these intertwined pathways hold promise for disease modification.
Study Design
Two recent pivotal studies investigated the hepatoprotective effects of linarin, a natural flavonoid glycoside commonly found in traditional herbal medicines with known anti-inflammatory, antioxidant, and hepatoprotective properties, focusing on its mechanisms against high-fat diet (HFD)-induced NAFLD and hepatic steatosis models.
The first study by Lv et al. explored linarin’s effects on NAFLD through modulation of the PI3K/Akt/mTOR signaling pathway, autophagy, and gut microbiota. In vitro, the NAFLD model employed AML12 mouse hepatocyte cells stimulated with oleic acid and palmitic acid to mimic lipid overload. In vivo, C57BL/6J mice were fed an HFD to induce chronic NAFLD. Key endpoints included lipid accumulation (Oil Red O and H&E staining), autophagy markers, inflammatory cytokine levels, and gut microbiota composition by 16S rRNA sequencing.
The second study by Xiao et al. investigated linarin’s role in inhibiting phosphodiesterase 4D (PDE4D) and activating the cAMP/PKA/CREB signaling cascade to ameliorate MAFLD features in HFD-fed C57BL/6J mice. Various linarin doses (50 and 100 mg/kg) were administered, with in vitro experiments in HepG2, AML12, and mouse primary hepatocytes exposed to oleic/palmitic acid. Outcomes measured were hepatic triglyceride content, oxidative stress markers, insulin sensitivity, and liver function parameters. Mechanistic assays included PDE4D activity and downstream pathway protein expression analysis.
Key Findings
Linarin Modulates PI3K/Akt/mTOR Pathway and Enhances Autophagy
Lv and colleagues reported that linarin significantly reduced intracellular lipid accumulation in AML12 cells and HFD-induced hepatic steatosis in mice. This effect correlated with upregulated autophagy, evidenced by increased LC3-II and Beclin-1, and reduced p62 expression. Mechanistic studies revealed that linarin inhibited the phosphorylation of PI3K, Akt, and mTOR, key negative regulators of autophagy, thereby activating autophagic flux to facilitate lipid clearance. Concurrently, linarin attenuated hepatic inflammatory responses by lowering proinflammatory cytokines such as TNF-α and IL-6.
Restoration of Gut Microbiota Balance
Gut microbiota profiling demonstrated that linarin reversed HFD-induced dysbiosis by decreasing the relative abundance of Firmicutes and Bacteroidetes, phyla implicated in obesity and metabolic dysfunction. Additionally, beneficial genera including Akkermansia and Bifidobacterium were increased, which may contribute to improved gut barrier function and systemic metabolic effects.
Inhibition of PDE4D and Activation of cAMP/PKA/CREB Pathway
Xiao et al. found that linarin exerts a complementary, distinct hepatoprotective mechanism by inhibiting PDE4D, reducing its activity that otherwise degrades cAMP. This elevated intracellular cAMP levels, activating the protein kinase A (PKA)/cAMP response element-binding protein (CREB) pathway, pivotal in lipid metabolism regulation. Activation of this pathway enhanced GPX4 expression, promoting antioxidant defense and reducing reactive oxygen species (ROS) and lipid peroxidation (MDA levels). Linarin also increased ATP production and endogenous antioxidant enzymes (GSH, CAT), mitigating mitochondrial dysfunction and oxidative stress.
In vivo, linarin-treated mice exhibited reduced weight gain, diminished hepatic fat accumulation, improved insulin sensitivity, and normalized liver enzyme levels (ALT/AST), underpinning metabolic improvements.
Expert Commentary
Emerging evidence supports linarin as a multifaceted agent capable of targeting several major pathophysiological axes in NAFLD. The convergence of findings from these robust in vitro and in vivo studies highlights dual mechanisms: modulation of autophagy/inflammation via PI3K/Akt/mTOR pathway suppression and enhancement of lipid metabolism and oxidative resistance through PDE4D inhibition and cAMP/PKA/CREB signaling activation.
Importantly, these studies underline the integral role of gut microbiota as a modifiable contributor to NAFLD pathogenesis and therapeutic response, with linarin demonstrating a capacity to correct dysbiosis.
While these preclinical findings are promising, clinical translation requires caution. Dose identification, pharmacokinetics, long-term safety, and efficacy in diverse human populations remain to be established. Additionally, interaction with existing metabolic and hepatic medications warrants investigation. Nonetheless, therapeutics like linarin that intervene upstream in fundamental signaling and metabolic pathways may offer superior disease modification potential compared to symptom-focused treatments.
Conclusion
Linarin presents a compelling candidate for NAFLD intervention through multi-targeted actions: promoting autophagy and reducing inflammation via PI3K/Akt/mTOR pathway inhibition, restoring gut microbiota homeostasis, and enhancing lipid metabolism and antioxidant capacity by PDE4D inhibition and cAMP/PKA/CREB pathway activation. These mechanistic insights pave the way for future clinical research and development of linarin and related flavonoids as natural, well-tolerated therapeutic options to combat the growing burden of fatty liver disease.
Ongoing studies should focus on detailed pharmacodynamics, rigorous clinical trials, and formulation strategies to optimize bioavailability. Integration of gut microbiome modulation with intracellular signaling correction signals a promising holistic approach in metabolic liver disease management.
References
Lv M, Zhai Y, Yu H, Cheng J, Wei Y, Zhang Y, Zhang Y, Feng H. Linarin alleviates high-fat diet-induced NAFLD via modulating the PI3K/Akt/mTOR pathway, autophagy, and gut microbiota. Biochim Biophys Acta Mol Cell Biol Lipids. 2025 Oct;1870(7):159666. doi: 10.1016/j.bbalip.2025.159666
Xiao Y, Wang J, Zhang H, Yang X, Zhou J, Zhou Y, Liu S, Liu M, Wang Y, Wang Y, Liao Q, Hou M, Hao Y, Liu S, Luo Z, Zhang S, Yu J, Yu L, Zhou L, Li Y, Li G. Linarin alleviates high-fat diet-induced hepatic steatosis by inhibiting PDE4D and activating the cAMP/PKA/CREB pathway. Free Radic Biol Med. 2025 Jul 23;239:116-129. doi: 10.1016/j.freeradbiomed.2025.07.030. Epub ahead of print. PMID: 40712988.