Background
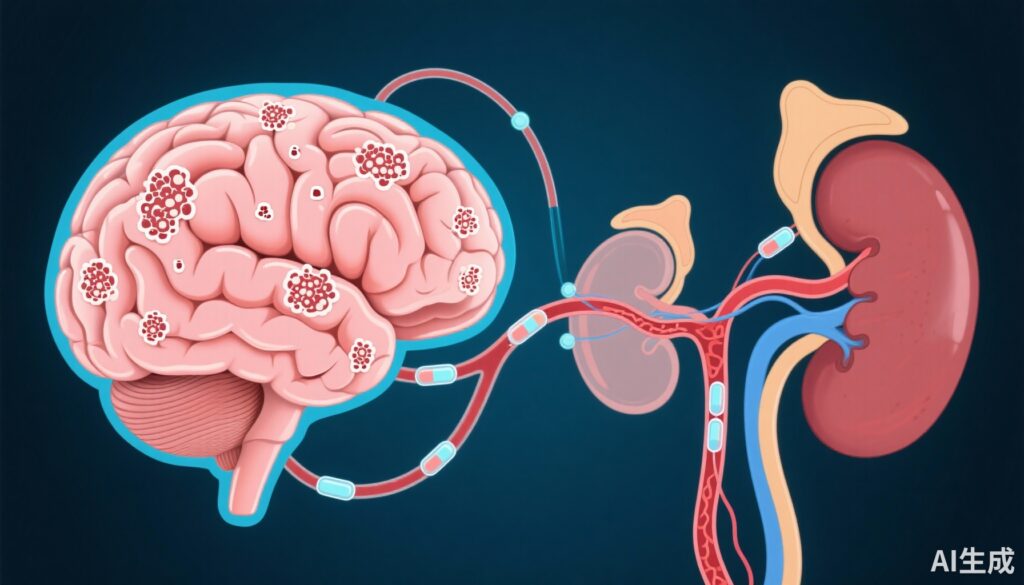
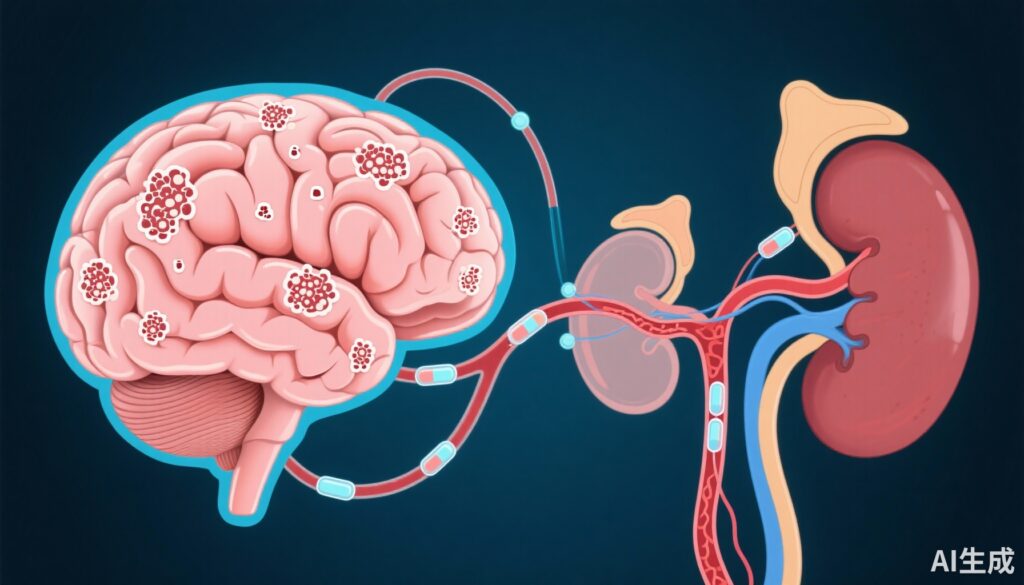
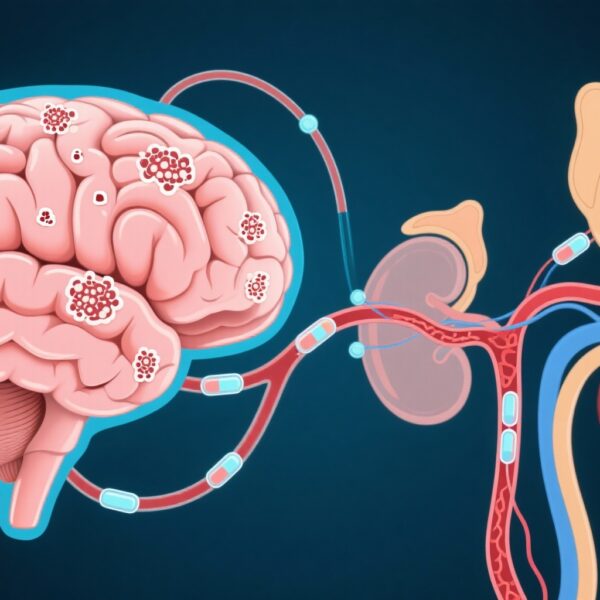
Alzheimer’s disease (AD) remains a leading cause of dementia worldwide, with its diagnosis increasingly supported by accurate blood-based biomarkers reflecting underlying neuropathology. These biomarkers include amyloid-β peptides (Aβ42, Aβ40), phosphorylated tau isoforms, and neurodegeneration markers such as neurofilament light chain (NfL) and glial fibrillary acidic protein (GFAP). However, comorbid systemic conditions, particularly kidney dysfunction, may confound blood biomarker levels due to altered metabolism and clearance. Given the widespread use of blood biomarkers in clinical AD diagnostic workflows, understanding the impact of renal function on biomarker levels and their predictive value for amyloid pathology is critical for precision medicine.
Study Design
This investigation analyzed 242 participants from the Translational Biomarkers in Aging and Dementia (TRIAD) cohort, encompassing cognitively unimpaired controls (n=124), mild cognitive impairment (MCI, n=58), Alzheimer’s disease dementia (n=34), and non-AD dementia cases (n=26). All participants underwent amyloid PET imaging with [18F] AZD-4694 to establish cerebral amyloid-β status. Plasma was analyzed using ultra-sensitive Simoa assays to quantify Aβ42, Aβ40, phosphorylated tau isoforms p-tau181, p-tau217, p-tau231, N-terminal tau fragments (NTA-tau), GFAP, and NfL.
Kidney function was evaluated using estimated glomerular filtration rate (eGFR, mL/min/1.73 m2), calculated via plasma creatinine alongside age and sex. Participants were stratified by chronic kidney disease (CKD) stages 1 to 3 based on eGFR thresholds. Linear regression models assessed associations between eGFR and each blood biomarker. Logistic regression models evaluated whether incorporating eGFR improved amyloid-β positivity prediction beyond biomarker levels and demographic covariates.
Key Findings
Concentrations of blood biomarkers were generally elevated in participants with CKD stage 3, followed by those with stages 2 and 1. Statistically significant differences across CKD stages were observed for plasma NfL, Aβ42, and Aβ40, but not for the Aβ42/Aβ40 ratio. Linear analyses revealed significant inverse associations of eGFR with most biomarkers except NTA-tau, indicating that lower kidney function correlates with higher biomarker concentrations, especially for Aβ40 and NfL.
Adjustment for age, sex, or amyloid PET standardized uptake value ratio (SUVr) attenuated the relationships markedly, with significant associations persisting only for Aβ40, Aβ42, NfL, and GFAP. This suggests that demographic factors and brain amyloid burden partially confound the kidney function–biomarker link.
Critically, incorporating eGFR into predictive models for amyloid-β positivity did not improve model fit or discriminative accuracy beyond the inclusion of plasma biomarkers, age, and sex. While age and sex significantly enhanced prediction, the addition of renal function parameters did not confer meaningful clinical benefit as evaluated by Akaike Information Criterion and area under the receiver operating characteristic curve.
Expert Commentary
This study provides nuanced insight into the influence of renal function on AD blood biomarkers. The observed elevations in protein biomarker concentrations among individuals with impaired kidney function likely reflect reduced systemic clearance rather than increased neurodegeneration per se. However, the loss of significance after key covariate adjustments reinforces that kidney function’s confounding effect is modest for most biomarkers when interpreted in context.
Importantly, blood biomarkers with highest diagnostic accuracy for AD pathology, such as p-tau217, were unaffected by eGFR, underscoring their robustness. These findings align with the biological plausibility that certain low molecular weight proteins filtered by the kidney may accumulate in plasma when renal function declines. The potential for kidney dysfunction to inflate levels of general neurodegeneration markers like NfL should be considered when clinical phenotyping is ambiguous.
Limitations include the relatively preserved renal function spectrum in the cohort, restricting conclusions about moderate to severe kidney disease. Future studies including broader CKD severity are warranted. Additionally, longitudinal assessment of biomarker dynamics in relation to progressive kidney impairment could better elucidate causal mechanisms.
Conclusions
This rigorous evaluation establishes that mild to moderate reductions in kidney function are associated with higher plasma concentrations of select AD biomarkers, notably Aβ40, Aβ42, NfL, and GFAP. Nevertheless, after controlling for demographic factors and amyloid burden, these associations diminish, and crucially, accounting for renal function does not improve clinical prediction of amyloid-β positivity.
Therefore, renal function within normal to mildly impaired ranges does not substantially compromise the clinical utility of plasma AD biomarkers, particularly those with high specificity such as p-tau217. This supports the practical application of blood-based biomarker assays in memory clinics without necessitating routine renal adjustment, although awareness of kidney function remains prudent when interpreting quantitative values.
Funding and Trial Registration
The study was supported by grants and institutional funding as detailed in the original publication. No registered clinical trial number was specified.
References
Arslan B, Brum WS, Pola I, Therriault J, Rahmouni N, Stevenson J, Servaes S, Tan K, Vitali P, Montembeault M, Klostranec J, Macedo AC, Tissot C, Gauthier S, Lantero-Rodriguez J, Zimmer ER, Blennow K, Zetterberg H, Rosa-Neto P, Benedet AL, Ashton NJ. The impact of kidney function on Alzheimer’s disease blood biomarkers: implications for predicting amyloid-β positivity. Alzheimers Res Ther. 2025 Feb 19;17(1):48. doi: 10.1186/s13195-025-01692-z. PMID: 39972340; PMCID: PMC11837363.