Background
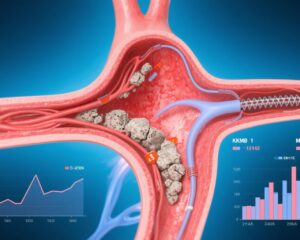
Acute myocardial infarction (MI) remains a leading cause of morbidity and mortality worldwide. Anemia frequently complicates acute MI, necessitating decisions regarding red blood cell (RBC) transfusion. The MINT trial (Myocardial Ischemia and Transfusion), involving 3,504 patients with MI and hemoglobin levels ≤10 g/dL, compared liberal (maintaining hemoglobin ≥10 g/dL) versus restrictive (maintaining hemoglobin ≥8 g/dL) RBC transfusion strategies. Initial findings suggested that liberal transfusion reduced the composite risk of 30-day death or recurrent MI. However, the impact of transfusion strategy specifically in patients undergoing revascularization (percutaneous coronary intervention or coronary artery bypass grafting) during the index hospitalization remained unclear. This subgroup analysis aimed to address that clinical uncertainty, enhancing guidance on transfusion in this high-risk population.
Study Design
This prespecified post hoc analysis of the MINT trial stratified participants based on whether they underwent revascularization prior to randomization but during the index hospitalization (n=1,002) or not (n=2,442). Participants had acute MI complicated by anemia (hemoglobin ≤10 g/dL). They were randomized to either liberal transfusion (maintaining hemoglobin ≥10 g/dL) or restrictive transfusion (maintaining hemoglobin ≥8 g/dL). The primary endpoint was the composite of 30-day all-cause death or MI. Secondary endpoints included 30-day all-cause death, recurrent MI alone, a composite of death, recurrent MI, ischemia-driven unscheduled revascularization or readmission for ischemic cardiac diagnosis, heart failure, and cardiac death. Multivariable log-binomial regression evaluated the relative risks (RR) of outcomes by transfusion strategy, incorporating interaction terms to assess whether revascularization status modified the treatment effect.
Key Findings
Patients undergoing revascularization were generally younger, more frequently female, and had fewer comorbid conditions compared to those who did not undergo revascularization. Examination of the primary outcome showed no statistically significant interaction between revascularization status and transfusion strategy—indicating that the effect of liberal versus restrictive transfusion on 30-day death or MI did not differ meaningfully between the groups.
However, an important exception was cardiac death. Restrictive transfusion was associated with a significantly increased risk of 30-day cardiac death among patients who did not undergo revascularization (RR 2.45; 95% CI 1.58–3.81), whereas among those who underwent revascularization, the risk of cardiac death was not significantly different between transfusion strategies (RR 0.97; 95% CI 0.59–1.60). The interaction term for cardiac death was statistically significant (P=0.006), suggesting revascularization status modifies the relationship between transfusion strategy and cardiac mortality.
Secondary outcomes including recurrent MI and composite ischemic events did not show significant interaction effects by revascularization status.
Expert Commentary
These results provide valuable insight into transfusion management in acute MI patients with anemia. The absence of interaction for most outcomes suggests a broadly consistent effect of transfusion strategy regardless of revascularization. Notably, the increased risk of cardiac death with restrictive transfusion among nonrevascularized patients may reflect vulnerability stemming from persistent ischemia, anemia-induced hypoxia, or a higher prevalence of comorbidities in this subgroup.
Existing clinical guidelines have favored restrictive transfusion thresholds in cardiovascular patients to avoid transfusion-related complications, but this study highlights that such an approach may not be optimal for all subgroups, particularly patients with acute MI who are managed conservatively without revascularization.
Limitations include the observational nature of subgroup comparisons and potential residual confounding despite multivariable adjustment. Further confirmatory randomized data focusing on the nonrevascularized population would be instrumental. Mechanistically, liberal transfusion may improve myocardial oxygen delivery and reduce ischemic stress, especially in patients not receiving mechanical restoration of coronary blood flow.
Conclusions
In this prespecified analysis of the MINT trial, revascularization did not significantly alter the impact of liberal versus restrictive RBC transfusion strategies on the composite outcome of 30-day death or MI in patients with acute MI and anemia. However, restrictive transfusion was associated with an increased risk of cardiac death in patients who did not undergo revascularization, a finding that warrants further validation. Clinicians should carefully consider revascularization status when individualizing transfusion strategies in this population.
References
Rao SV, Brooks MM, D’Agostino HEA, Steg PG, Simon T, Aronow HD, Goldsweig AM, Malik S, Alsweiler C, Ho KKL, Dehghani P, Caixeta A, Quraishi AR, Robinson S, Traverse JH, Siddiqi O, Fergusson DA, Potter BJ, Schulman-Marcus J, Keating FK, Carson JL; MINT Trial Investigators. Effect of Red Blood Cell Transfusion Strategy on Clinical Outcomes Among Patients With Acute Myocardial Infarction Undergoing Revascularization: A Prespecified Analysis of the MINT Trial. Circ Cardiovasc Interv. 2025 May;18(5):e015249. doi: 10.1161/CIRCINTERVENTIONS.125.015249. Epub 2025 Mar 30. PMID: 40159118; PMCID: PMC12092174.
ClinicalTrials.gov. Myocardial Ischemia and Transfusion (MINT) Trial. NCT02981407. https://clinicaltrials.gov/ct2/show/NCT02981407