Highlights of the Three-Decade Brussels Experience
During a median follow-up of 103 months, 14% of patients with Brugada Syndrome (BrS) experienced at least one sustained ventricular arrhythmia (VA), equating to 1.59 events per 100 person-years. While the implantable cardioverter-defibrillator (ICD) remains the cornerstone of sudden cardiac death (SCD) prevention, device-related complications are substantial, with 27% of patients requiring device revision or lead replacement. Thoracoscopic epicardial ablation has emerged as a significant adjunctive therapy, demonstrating a marked reduction in ventricular events among high-risk cohorts.
Introduction: The Brugada Conundrum
Since its formal description in 1992, Brugada Syndrome (BrS) has remained one of the most challenging inherited primary arrhythmia syndromes for clinical management. Characterized by ST-segment elevation in the right precordial leads and an increased risk of sudden cardiac death (SCD) in the absence of structural heart disease, BrS often affects young, otherwise healthy individuals. For three decades, the implantable cardioverter-defibrillator (ICD) has served as the definitive therapy for those at high risk. However, the long-term management of these patients—many of whom receive their first device in their 20s or 30s—presents a complex clinical trajectory defined by the need for repeated generator changes, lead failures, and the psychological impact of inappropriate shocks.
Study Design and Population Dynamics
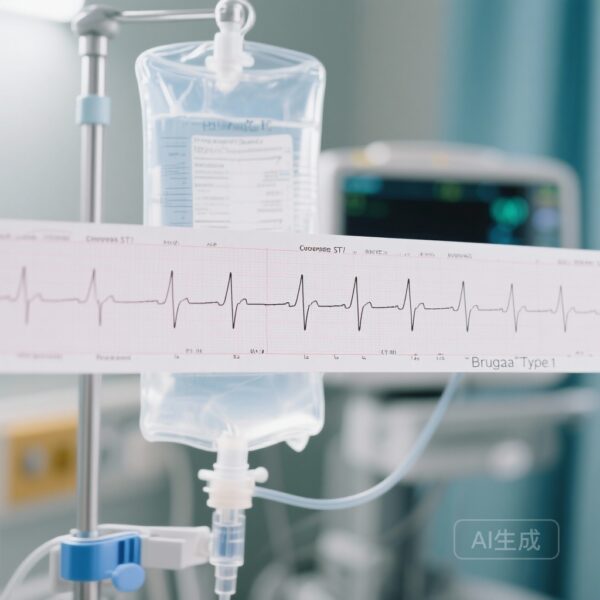
In a landmark study published in JACC: Clinical Electrophysiology, Monaco and colleagues detailed a 30-year single-center experience from the University Hospital Brussels, a pivotal center in BrS research. The study prospectively enrolled 306 consecutive patients (61% male; mean age 41 ± 17 years) who received ICDs between 1992 and 2022. The inclusion criteria required a Type 1 Brugada ECG pattern (either spontaneous or drug-induced) and consistent clinical follow-up.
Risk stratification evolved over the study period. While early years relied on symptomatic status and family history, the latter part of the study (from 2017) utilized the multiparametric Brussel risk score. This score integrates clinical variables such as spontaneous Type 1 ECG, syncope, sinus node dysfunction, and electrophysiological study (EPS) results to more accurately identify candidates for primary prevention. Notably, 16% of the cohort received ICDs for secondary prevention (survivors of cardiac arrest or sustained VA), while the remainder were primary prevention implants.
Long-Term Outcomes: Arrhythmic Events and Survival
The study provides critical data on the natural history of BrS in protected populations. Over the 30-year period, 14% of the total cohort experienced sustained VAs. The incidence was significantly higher in the secondary prevention group compared to the primary prevention group, underscoring the high recurrence risk in those who have already manifested life-threatening arrhythmias.
Genetic factors and prior clinical history were strong predictors of future events. Loss-of-function mutations (primarily in SCN5A) and the presence of prior non-sustained ventricular arrhythmias were independently associated with the occurrence of sustained VAs during follow-up. Interestingly, patients in the secondary prevention group also showed a higher incidence of supraventricular arrhythmias, suggesting a broader substrate for electrical instability in these individuals.
Overall mortality was 5.88%, but only 22.2% of these deaths were attributed to cardiac causes. This suggests that in centers with expert management and appropriate ICD utilization, the risk of SCD can be effectively mitigated, shifting the clinical focus toward managing the long-term sequelae of the therapy itself.
The Burden of Technology: Complications and Inappropriate Shocks
Perhaps the most sobering findings of the Monaco et al. study involve the technical challenges of long-term ICD therapy. In a population with a median age of 41 at first implant, the cumulative “device mileage” is immense. The study reported that 27% of patients required some form of device revision or lead replacement. Lead failure and insulation issues remain the Achilles’ heel of transvenous ICD systems, particularly in younger, more active patients.
Inappropriate shocks occurred in 15% of patients. Contrary to some clinical assumptions, the presence of single versus dual-chamber leads did not significantly affect the rate of inappropriate shocks. These events are often triggered by sinus tachycardia, supraventricular arrhythmias, or T-wave oversensing, and they carry a significant psychological burden, sometimes leading to post-traumatic stress or avoidance behaviors in patients.
A Paradigm Shift: Epicardial Ablation
A transformative element of the study is the integration of video-thoracoscopic epicardial ablation, which the center began performing in 2016 for high-risk patients. The rationale for this approach stems from the identification of the right ventricular outflow tract (RVOT) epicardium as the primary site of the arrhythmogenic substrate in BrS.
In the high-risk cohort, those who underwent epicardial ablation experienced significantly fewer ventricular events compared to those managed with ICD therapy alone. This suggests that ablation may not only be an adjunctive therapy for those with frequent shocks but could potentially play an earlier role in the treatment algorithm to reduce the overall arrhythmic burden and the subsequent need for ICD interventions.
Clinical Implications and Expert Commentary
The findings from this 30-year cohort emphasize that while the ICD is a lifesaving tool, it is not a “set and forget” solution. The high rate of revisions and inappropriate shocks in BrS patients demands a more nuanced approach to risk stratification. The use of the Brussel risk score represents a move toward this precision, aiming to avoid over-implantation in low-risk asymptomatic patients while ensuring that those at high risk are protected.
Furthermore, the success of epicardial ablation highlights a shift in the treatment philosophy from reactive (shocking an arrhythmia) to proactive (modifying the substrate). For clinicians, this means that the management of BrS should be multidisciplinary, involving electrophysiologists skilled in both device management and advanced ablation techniques.
Limitations of the study include its single-center nature and the evolution of technology and guidelines over three decades, which may introduce historical bias. However, the sheer duration of follow-up and the consistency of the clinical setting provide an invaluable longitudinal perspective that multi-center, short-term trials often lack.
Conclusion
ICD therapy remains the definitive safeguard against sudden cardiac death in Brugada Syndrome, particularly for secondary prevention. However, the high incidence of device-related complications and inappropriate shocks over 30 years highlights the need for individualized treatment strategies. The integration of epicardial ablation offers a promising avenue to reduce arrhythmic risk and improve the long-term quality of life for these patients. As we move into the fourth decade of Brugada research, the focus must remain on refining risk prediction and optimizing the balance between the protective benefits of technology and its inherent clinical costs.