Highlights
- Over a median follow-up of 13.2 years, primary prevention ICD implantation did not significantly reduce the rate of all-cause mortality in patients with nonischemic heart failure with reduced ejection fraction (HFrEF).
- ICD implantation was associated with a significant 46% reduction in the risk of sudden cardiovascular death (HR: 0.54; 95% CI: 0.36-0.80).
- Age remains a critical determinant of benefit; patients aged 70 years or younger derived a substantial reduction in sudden death (HR: 0.38), whereas those over 70 did not.
- Secondary analyses suggest that frailty and atrial fibrillation (AF) may influence cardiovascular outcomes, but they do not negate the primary findings regarding ICD efficacy.
Background: The Evolution of Nonischemic HFrEF Management
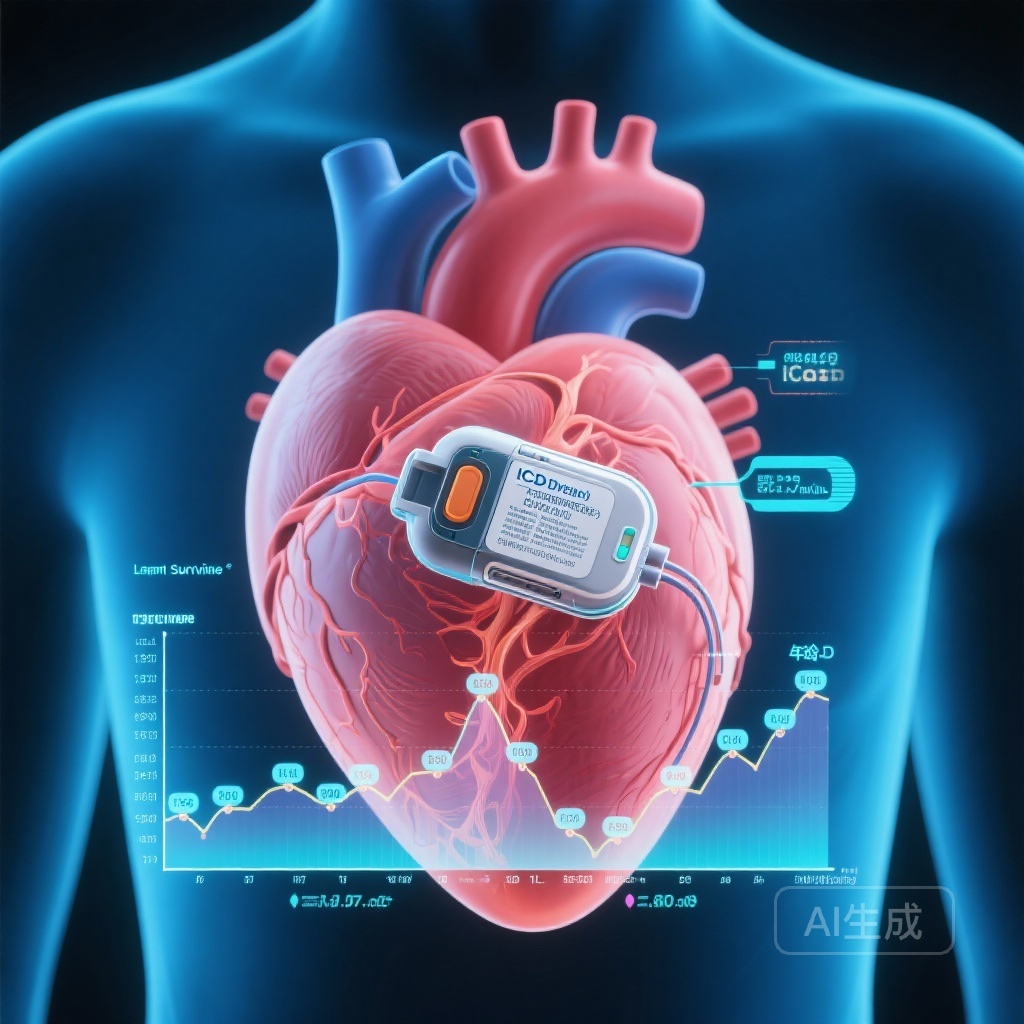
The role of the implantable cardioverter-defibrillator (ICD) in the primary prevention of sudden cardiac death (SCD) has been a cornerstone of heart failure management for decades. While the evidence supporting ICD use in ischemic heart disease is robust, its application in nonischemic systolic heart failure has historically been more controversial. Early landmark trials, such as SCD-HeFT, suggested a benefit across the spectrum of heart failure etiologies, but these findings were often based on subgroup analyses conducted in an era before the widespread adoption of contemporary guideline-directed medical therapy (GDMT), including sacubitril/valsartan, SGLT2 inhibitors, and advanced cardiac resynchronization therapy (CRT).
As the management of HFrEF has improved, the absolute risk of sudden cardiac death has declined, while the risk of death from pump failure or non-cardiovascular causes has remained significant, particularly in aging populations. This shift in the competing risks of death necessitates a re-evaluation of long-term ICD efficacy. The Danish Study to Assess the Efficacy of ICDs in Patients with Non-ischemic Systolic Heart Failure on Mortality (DANISH) was designed to address this gap, and its extended follow-up provides unprecedented insight into the life-cycle of ICD benefit in this specific patient population.
Study Design: The DANISH Trial Framework
The DANISH trial was a multi-center, randomized, controlled trial that enrolled 1,116 patients with symptomatic nonischemic HFrEF. Inclusion criteria required a left ventricular ejection fraction (LVEF) of 35% or less, NYHA functional class II or III (or class IV if CRT was planned), and elevated levels of N-terminal pro-B-type natriuretic peptide (NT-proBNP). Patients were randomized 1:1 to receive either a primary prevention ICD or usual clinical care. Notably, 58% of patients in both groups received CRT, reflecting a modern heart failure cohort.
The primary endpoint was all-cause mortality. Secondary endpoints included cardiovascular death and sudden cardiovascular death. In the extended follow-up analysis, the median observation period reached 13.2 years (Q1-Q3: 11.6-14.6 years), allowing researchers to observe how the early trends in the data matured over more than a decade of clinical progress.
Key Findings: Long-Term Outcomes and Mode of Death
All-Cause Mortality and the Competing Risk Phenomenon
During the extended follow-up, 294 patients (52.9%) in the ICD group and 299 (53.4%) in the control group died. The analysis showed that ICD implantation did not significantly reduce the long-term rate of all-cause death (Hazard Ratio [HR]: 0.96; 95% CI: 0.82-1.13). This finding underscores a critical reality in modern heart failure care: as patients live longer with nonischemic HFrEF, they increasingly succumb to non-arrhythmic causes, such as progressive heart failure or non-cardiovascular comorbidities. The life-saving potential of an ICD—which only prevents death from tachyarrhythmias—is often diluted by these competing risks.
Significant Reduction in Sudden Cardiovascular Death
Despite the lack of an all-cause mortality benefit in the total population, the ICD remained highly effective at its primary physiological task. The trial reported a significant reduction in the long-term rate of sudden cardiovascular death (HR: 0.54; 95% CI: 0.36-0.80). This confirms that the device continues to provide protection against lethal arrhythmias over a decade after implantation, even in a nonischemic population receiving high-quality medical therapy.
Age as a Definitive Treatment Modifier
One of the most impactful findings from the DANISH trial is the interaction between age and ICD benefit. While the effect of ICDs on all-cause death appeared consistent across age groups (P-interaction = 0.89), age significantly modified the effect on sudden cardiovascular death (P-interaction = 0.01). In patients aged 70 years or younger, ICD implantation dramatically reduced the rate of sudden death (HR: 0.38; 95% CI: 0.23-0.62). Conversely, in patients older than 70 years, no such benefit was observed (HR: 1.27; 95% CI: 0.56-2.89).
This discrepancy is likely due to the higher burden of non-sudden death in older individuals. In the ≤70 age group, the rate of non-sudden death was 2.7 per 100 patient-years, whereas in the >70 group, it rose to 5.4 per 100 patient-years. For younger patients, sudden death represents a larger proportion of the total mortality risk, making the ICD a more impactful intervention.
Secondary Analyses: Frailty and Atrial Fibrillation
The Impact of Frailty
Recognizing that chronological age is not always a perfect proxy for biological health, the DANISH investigators also evaluated the impact of frailty using the Rockwood cumulative deficit approach. Patients were categorized into three frailty classes. While frailty was a strong predictor of overall mortality, it did not significantly modify the effect of ICD implantation on all-cause death (P-interaction = 0.99). Interestingly, the beneficial effect of ICDs on sudden cardiovascular death appeared potentially greater in more frail patients in some analyses, though this trend was not sustained when frailty was analyzed as a continuous variable. This suggests that while frailty increases overall risk, it should not automatically preclude ICD consideration if the patient is relatively young and has a high risk of arrhythmia.
The Role of Atrial Fibrillation
Atrial fibrillation (AF) was present in approximately 37.5% of the DANISH cohort at baseline. The presence of AF significantly modified the effect of ICD implantation on cardiovascular death (P-interaction = 0.04). Patients with AF who received an ICD had a lower rate of cardiovascular death (HR: 0.67) compared to those without AF (HR: 1.04). This suggests that AF may serve as a marker for a phenotype of heart failure that remains particularly susceptible to the benefits of rhythm protection, potentially due to the higher incidence of cardiovascular complications in this subgroup.
Expert Commentary: Clinical Implications
The long-term data from the DANISH trial provide a nuanced roadmap for clinicians. The primary takeaway is that the decision to implant an ICD in a patient with nonischemic HFrEF should not be reflexive but should instead be a personalized assessment of the patient’s specific risk profile. The ’70-year rule’ suggested by this data offers a practical clinical threshold. For younger patients, the ICD remains a vital tool for extending life by preventing sudden death. For older patients, the focus should perhaps shift toward optimizing GDMT and managing the comorbidities that contribute to non-sudden mortality.
Furthermore, the high rate of CRT use in the DANISH trial (nearly 60%) is significant. CRT itself reduces the risk of sudden death by improving ventricular function and reducing remodeling. The fact that the ICD provided additional sudden-death protection even in a CRT-heavy population highlights the persistent risk of ventricular arrhythmias in HFrEF, though it also raises the bar for proving an all-cause mortality benefit.
Conclusion
In summary, the 13.2-year follow-up of the DANISH trial confirms that primary prevention ICD implantation in nonischemic HFrEF does not reduce all-cause mortality across the entire population but provides a durable and significant reduction in sudden cardiovascular death. The benefit is most pronounced in younger patients (≤70 years), who have fewer competing risks of death. Clinicians should use these findings to engage in shared decision-making, particularly for older or frailer patients where the risk-benefit ratio of device implantation is less clear.
Funding and ClinicalTrials.gov Registration
The DANISH trial was funded by Medtronic, the Danish Council for Strategic Research, the Danish Heart Foundation, and other regional health authorities in Denmark. ClinicalTrials.gov Identifier: NCT00542945.
References
- Butt JH, et al. Long-Term Effect of ICDs in Nonischemic Heart Failure With Reduced Ejection Fraction: Extended Follow-Up Analysis of DANISH. J Am Coll Cardiol. 2025 Dec 16;86(24):2402-2414.
- Køber L, et al. Defibrillator Implantation in Patients with Nonischemic Systolic Heart Failure. N Engl J Med. 2016 Sep 29;375(13):1221-30.
- Butt JH, et al. Implantable Cardioverter-Defibrillator and Frailty in Non-ischemic Heart Failure With Reduced Ejection Fraction: Extended Follow-Up of the DANISH Trial. Am J Cardiol. 2026 Jan 15;259:163-172.
- Elming MB, et al. Age and Outcomes of Primary Prevention Implantable Cardioverter-Defibrillators in Patients With Nonischemic Systolic Heart Failure. Circulation. 2017 Nov 7;136(19):1772-1780.
- Doi SN, et al. Atrial fibrillation and implantable cardioverter-defibrillator in non-ischaemic heart failure with reduced ejection fraction: insights from the DANISH trial. Europace. 2025 Sep 1;27(9):euaf200.