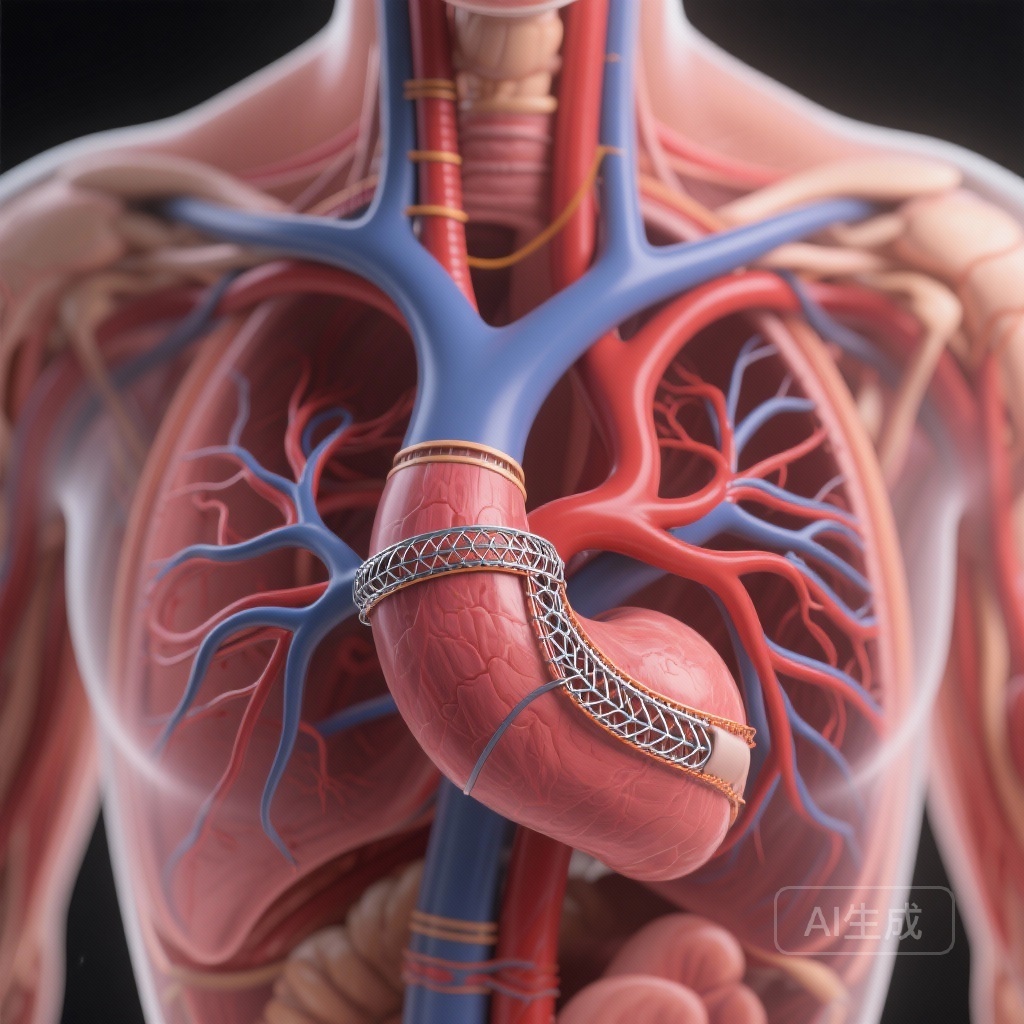
Introduction: The Frontier of Total Endovascular Arch Repair
The management of aortic arch pathologies remains one of the most formidable challenges in cardiovascular surgery. While open surgical repair involving deep hypothermic circulatory arrest has long been the gold standard, its associated morbidity and mortality—particularly in elderly patients with multiple comorbidities—have driven the development of less invasive alternatives. Total endovascular arch repair (TEVAR) using custom-made branched stent grafts has emerged as a promising solution for high-risk patients. However, the success of these procedures is heavily dependent on the anatomical characteristics of the proximal landing zone, specifically the native ascending aorta (Zone 0).
In clinical practice, a dilated ascending aorta is often viewed with caution by vascular surgeons. When the diameter exceeds 38 mm, the mechanical stresses on the stent graft and the underlying vessel wall increase significantly. A recent two-center observational study by Wan et al., published in the European Journal of Vascular and Endovascular Surgery, provides a sobering look at the outcomes of endovascular arch repair in this specific patient population.
Highlighting Key Study Insights
Technical Feasibility vs. Clinical Success
The study reports a high technical success rate of 96%, indicating that current custom-made branched devices can be successfully deployed even in dilated anatomies. However, this technical success did not translate into favorable clinical outcomes, as evidenced by a 40% 30-day mortality rate.
The Risk of Retrograde Type A Dissection
Retrograde Type A dissection (RTAD) remains a catastrophic complication. In this cohort, RTAD was observed in 12% of cases, contributing significantly to the early mortality observed in the first post-operative week.
Neurological Complications
Despite advances in cerebral perfusion and device design, the total stroke rate (major and minor) reached 20%, underscoring the ongoing risk of embolic events during complex arch manipulations in dilated vessels.
Study Design and Patient Population
This retrospective observational study pooled data from two high-volume vascular centers between July 2018 and April 2025. The investigators identified 211 patients treated with arch branch devices, of whom 25 (14%) met the inclusion criteria of having a native ascending aorta diameter greater than 38 mm.
The cohort had a median age of 68.88 years, with a predominance of male patients (68%). The mean diameter of the ascending aorta was 41.28 ± 2.94 mm. The primary indications for intervention included thoracic aortic aneurysms (76%), aortic dissections (12%), and penetrating atherosclerotic ulcers (12%). Notably, 36% of these procedures were performed under urgent conditions, reflecting the high-stakes nature of treating symptomatic or rapidly expanding arch pathologies in patients deemed unfit for open surgery.
Detailed Analysis of Results
Early Clinical Outcomes
The primary finding of the study is the high 30-day mortality rate of 40%. When stratified by the urgency of the procedure, mortality was 24% (n=6) for elective cases and 16% (n=4) for urgent cases. While one might expect higher mortality in urgent settings, the high baseline mortality in elective cases suggests that a dilated ascending aorta represents an independent risk factor for poor outcomes in endovascular arch repair.
The causes of death were predominantly aortic-related. These included three cases of RTAD and two cases of cardiac tamponade. Other causes included myocardial infarction (n=2), stroke, and pulmonary embolism. The majority of these fatalities occurred within the first seven days following the procedure, highlighting the criticality of the immediate post-operative window.
Morbidity and Neurological Events
Neurological safety is a paramount concern in arch interventions. The study reported major strokes in 8% of patients and minor strokes in 12%. Furthermore, spinal cord ischemia was observed in 12% (n=3) of cases. These figures are considerably higher than those reported in cohorts with narrower ascending aortas, suggesting that the dilated vessel may complicate catheter manipulation and increase the risk of plaque liberation or malperfusion.
Anatomical and Procedural Factors
The mean proximal oversizing of the stent grafts was 13%. In a dilated and often pulsatile ascending aorta, achieving a stable and durable seal is difficult. The “bird-beaking” phenomenon, where the proximal end of the graft does not conform to the lesser curvature of the arch, is more prevalent in wider vessels, potentially leading to endoleaks or vessel wall injury. Although no intra-operative type I or III endoleaks were reported in this series, the high rate of RTAD suggests that the radial force exerted by the oversized grafts on a fragile, dilated aortic wall may be a primary driver of vessel failure.
Expert Commentary: Navigating the Hostile Aorta
The results of this study serve as a critical warning for the vascular community. The ascending aorta is a dynamic environment, subject to high-velocity blood flow and significant longitudinal displacement during each cardiac cycle. When the diameter exceeds 38 mm, the mechanical mismatch between the rigid stent graft and the compliant aortic wall is exacerbated.
Experts suggest that the high mortality rate observed here should prompt a re-evaluation of patient selection criteria. For patients with an ascending aorta > 38 mm, open surgical repair—perhaps using a frozen elephant trunk technique—should be prioritized if the patient has any reasonable chance of surviving the surgery. The endovascular approach, while technically possible, appears to carry a prohibitive risk in this specific anatomical subgroup.
Furthermore, the high incidence of RTAD (12%) points toward a need for device optimization. Current endografts may require modifications in proximal tip design or material stiffness to better accommodate the geometry of a dilated Zone 0. Until such advancements are made, the use of custom-made branched devices in these patients should be reserved for cases where no other viable options exist, and even then, only after extensive multidisciplinary consultation.
Conclusion: A Call for Caution and Optimization
The study by Wan et al. demonstrates that while endovascular arch repair in patients with a native ascending aorta > 38 mm is technically feasible, it is associated with substantial early morbidity and mortality. The 40% 30-day mortality rate and the 12% rate of retrograde Type A dissection are significantly higher than benchmarks for standard arch repair.
These findings underscore several critical points for clinical practice:
Meticulous Patient Selection
Clinicians must weigh the risks of endovascular failure against the risks of open surgery. A diameter of 38 mm may represent a relative contraindication for current endovascular technologies in the arch.
The Importance of High-Volume Centers
These complex procedures should only be performed in specialized centers with extensive experience in both endovascular and open aortic surgery, ensuring that complications like RTAD can be managed emergently if possible.</n
Need for Technological Innovation
The high rate of aortic-related deaths suggests that current device designs are not yet optimized for the hemodynamics and geometry of a dilated ascending aorta. Continued research into graft compliance and fixation mechanisms is essential.
In summary, while endovascular therapy continues to push the boundaries of what is treatable, the dilated ascending aorta remains a “hostile” landing zone. For now, a cautious approach, emphasizing open repair where feasible and rigorous planning where not, remains the safest path forward for patients with complex arch pathology.
References
1. Wan Z, Jama K, Hasemaki N, et al. Outcomes after Endovascular Arch Repair in Patients with Native Ascending Aorta Diameter Greater than 38 mm: An Observational Study in Two High Volume Centres. Eur J Vasc Endovasc Surg. 2026 Jan 17:S1078-5884(26)00056-0. doi: 10.1016/j.ejvs.2026.01.022.
2. Czerny M, et al. International expert consensus on the management of aortic arch diseases. Eur J Cardiothorac Surg. 2019;55(1):28-62.
3. Tsilimparis N, et al. Branched endovascular strategy for arch aneurysms: A multi-center experience. J Vasc Surg. 2020;71(2):351-359.