Highlight
- Both AV nodal and infranodal block occur after transcatheter aortic valve replacement (TAVR), but their timing and predictors differ markedly.
- Preexisting right bundle-branch block (RBBB) predicts intraprocedural heart block but not delayed heart block.
- Post-TAVR conduction parameters such as prolonged His-ventricular interval, PR interval, and AV Wenckebach cycle length strongly predict delayed block.
- Permanent pacemakers were required in nearly 10% of patients, underscoring the clinical impact of conduction complications.
Background
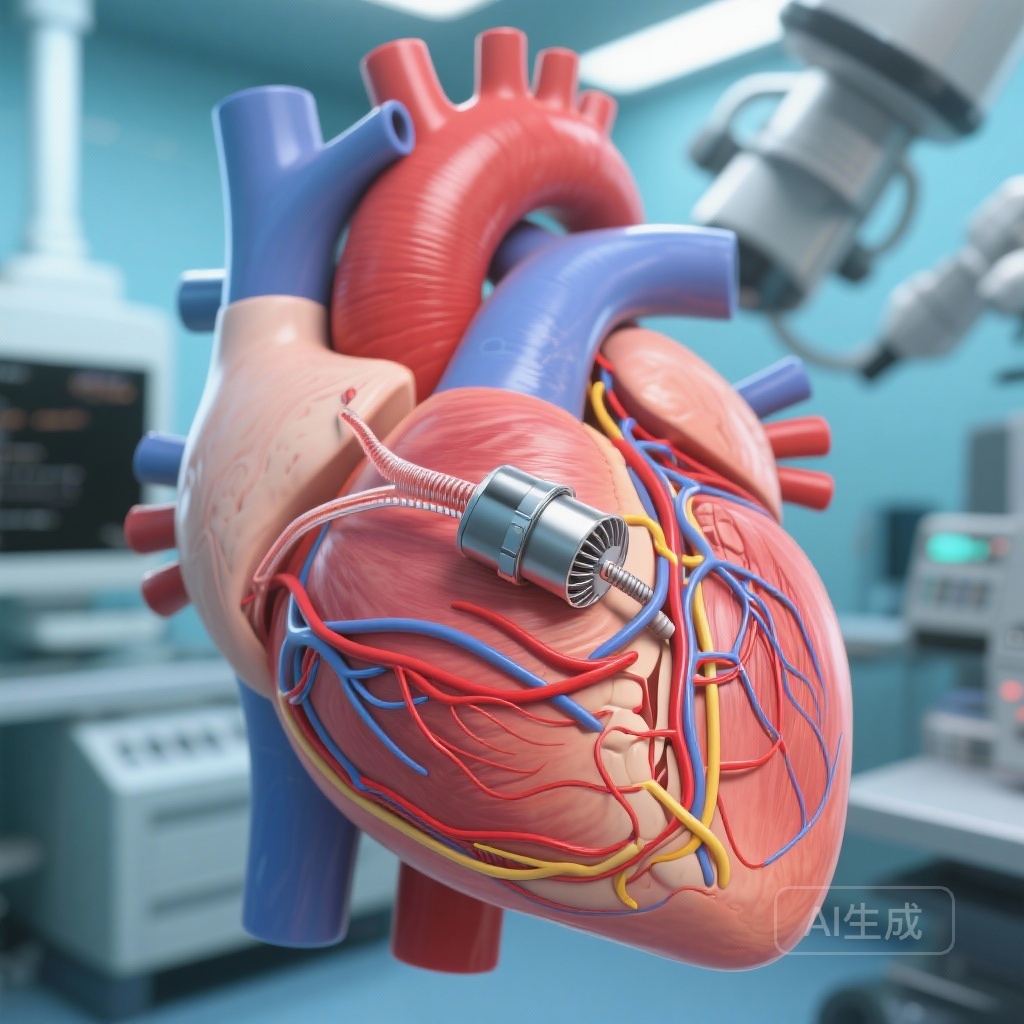
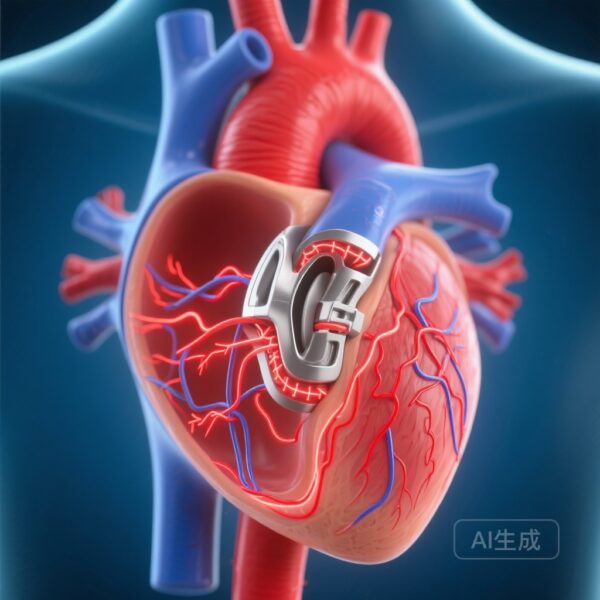
Severe aortic stenosis is a highly prevalent degenerative valve condition in elderly populations, often treated with transcatheter aortic valve replacement (TAVR) when surgical risk is high. While TAVR offers survival and symptomatic benefit, peri- and post-procedure heart block remains a significant concern, leading to a need for permanent pacemaker implantation in around 10–15% of cases. Conduction abnormalities after TAVR may occur immediately during valve deployment or be delayed, appearing days to weeks later. Understanding the electrophysiologic mechanisms underlying these conduction disturbances is key for risk stratification and refining operative techniques.
Study Design
This prospective cohort study was conducted at a single academic medical center in Boston, Massachusetts between May 2021 and January 2024. Four hundred nine consecutive patients undergoing TAVR were enrolled, excluding those with pre-existing pacemakers. At both the beginning and end of the procedure, a detailed electrophysiologic study was performed. Continuous monitoring included electrocardiography and His bundle recordings. In patients with preexisting RBBB or new conduction abnormalities, ECG monitoring continued after discharge. Patients were followed for one year to capture both immediate and delayed high-grade atrioventricular (AV) block, defined as Mobitz type II or complete heart block.
Key Findings
Of the 409 patients (median age 78.5 years, 44.5% female), 40 (9.7%) developed heart block requiring a permanent pacemaker. Fifteen cases emerged during the TAVR procedure, while 25 occurred afterward—within days to weeks. Persistent block was seen in all intraprocedural cases; in the post-TAVR group, most blocks were paroxysmal (20/25).
Electrophysiologic localization revealed that intraprocedural AV block was AV nodal in 6 cases (all transient and resolved during the procedure) and infranodal in 9 cases (non-resolving). Delayed block was AV nodal in only 3 patients (7.5%) and infranodal in the vast majority (22/25).
Predictors differed by timing: preexisting RBBB was the only significant predictor of intraprocedural block (but lacked predictive value for delayed block). Conversely, three post-procedure conduction parameters were strongly associated with delayed block: His-ventricular interval ≥80 milliseconds, PR interval ≥300 milliseconds, and AV Wenckebach cycle length ≥500 milliseconds.
These findings suggest distinct pathophysiologic pathways for early versus delayed conduction disturbances. Intraprocedural blocks may relate to mechanical trauma and immediate compression of the conduction tissue, while delayed infranodal blocks potentially reflect evolving edema, ischemia, or fibrotic remodeling following valve implantation.
Expert Commentary
The differentiation between AV nodal and infranodal mechanisms has critical implications. AV nodal block—more common intraprocedurally—may resolve spontaneously as procedural trauma subsides, whereas infranodal block—dominant in delayed presentations—is less likely to recover and often warrants permanent pacing. This aligns with histopathologic evidence of TAVR-induced injury near the interventricular septum and His-Purkinje fibers.
Pre-procedural recognition of high-risk anatomy and conduction patterns should guide patient counseling and decisions on early pacemaker placement versus prolonged observation. Continuous monitoring strategies, especially in patients with prolonged HV intervals or PR times post-TAVR, might prevent catastrophic bradyarrhythmias after discharge.
Limitations include single-center design, the lack of multi-center validation, and potential variation in valve type and operator practice influencing outcomes. Nonetheless, this rigorously monitored cohort provides important mechanistic insights.
Conclusion
This study demonstrates that the pathogenesis of AV block after TAVR is temporally and mechanistically heterogeneous. Early blocks often reflect AV nodal injury, while delayed blocks are usually infranodal, associated with measurable conduction delays at discharge. Incorporating electrophysiologic measurements into risk prediction models could improve post-TAVR surveillance and patient safety. Future multi-center studies should assess whether these findings generalize to varied populations and procedural techniques.
Funding and Registration
No external funding sources were reported. The study is registered and indexed under PMID: 41370050; PMCID: PMC12696659.
References
Waks JW, Poulin MF, Clarke JD, Pinto DS, d’Avila A, Tung P, Ultimo B, Guibone KA, Kiernan K, Medline A, Haouzi A, Rathakrishnan B, Abdel-Razek O, Laham RJ, Buxton AE. Mechanisms Underlying Alterations in Cardiac Conduction After Transcatheter Aortic Valve Replacement. JAMA Cardiol. 2025 Dec 10:e254442. doi:10.1001/jamacardio.2025.4442. Epub ahead of print. PMID: 41370050; PMCID: PMC12696659.