Highlights of the Study
Research published in the journal Stroke (2026) indicates that the use of Glucagon-Like Peptide-1 Receptor Agonists (GLP-1RAs) is associated with a 34% reduction in the risk of nontraumatic subarachnoid hemorrhage (SAH) among patients with intracranial aneurysms (IAs) and type 2 diabetes.
The protective effect remained consistent in a subgroup analysis of patients who had not received prior surgical or endovascular treatment for their aneurysms, showing a 32% risk reduction.
Beyond aneurysm-specific outcomes, GLP-1RA therapy was linked to a 37% reduction in all-cause mortality over a five-year follow-up period, reinforcing the systemic benefits of this drug class in high-risk populations.
A rigorous falsification analysis confirmed that these findings were unlikely to be driven by differences in healthcare access or the intensity of medical surveillance between the treatment and control groups.
Background: The Clinical Challenge of Intracranial Aneurysms
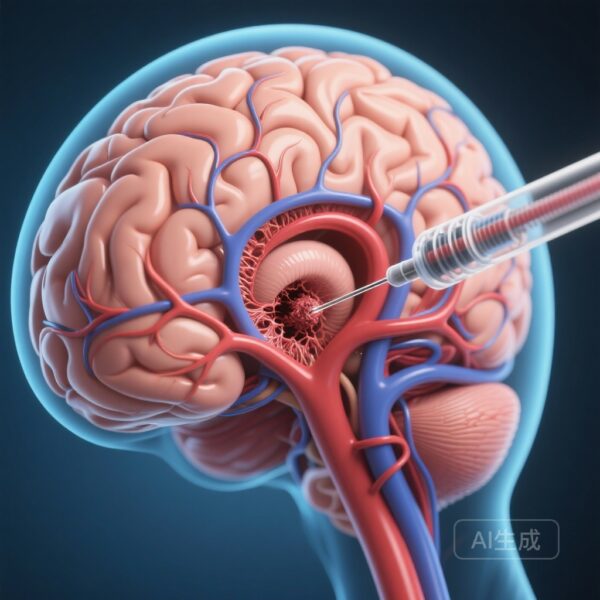
Intracranial aneurysms (IAs) are relatively common, affecting approximately 3% of the general population. While many remain asymptomatic, their rupture leads to subarachnoid hemorrhage (SAH), a catastrophic event associated with a 30% to 50% mortality rate and significant long-term disability in survivors. Currently, the management of unruptured IAs focuses on either surgical clipping, endovascular coiling, or conservative observation with serial imaging. However, there is a profound lack of evidence-based pharmacological therapies aimed at stabilizing the aneurysm wall or preventing rupture.
Recent scientific focus has shifted toward the role of chronic inflammation and vascular remodeling in the pathogenesis of aneurysm growth and eventual rupture. Glucagon-like peptide-1 receptor agonists (GLP-1RAs), originally developed for type 2 diabetes and obesity, have demonstrated remarkable pleiotropic effects beyond glycemic control. These include potent anti-inflammatory properties, improvements in endothelial function, and blood pressure regulation. Given that inflammation is a key driver of aneurysm wall degradation, researchers hypothesized that GLP-1RAs might provide a protective effect for patients harboring IAs.
Study Design and Methodology
To investigate this hypothesis, researchers conducted a retrospective cohort study utilizing the TriNetX database, a comprehensive global health research network. This database provided access to electronic health records from over 90 healthcare organizations across North America, South America, Europe, and Asia, representing a diverse and high-volume patient population. The study period spanned 15 years, from January 2010 to January 2025.
The study population included adult patients diagnosed with both type 2 diabetes and unruptured intracranial aneurysms. The primary exposure was the use of GLP-1RAs (n=2,517), which were compared against a control group of patients who did not receive these medications (n=23,431). To minimize the risk of confounding, the researchers employed 1:1 propensity score matching (PSM) based on 95 demographic and clinical variables. These variables included critical risk factors for aneurysm rupture such as age, sex, smoking status, hypertension, hyperlipidemia, and the use of other antihyperglycemic or antihypertensive medications.
The primary endpoints were the incidence of nontraumatic subarachnoid hemorrhage and all-cause mortality over a five-year follow-up period. A specific matched subgroup analysis was also performed on “untreated” patients—those who had no history of surgical or endovascular intervention—to isolate the medication’s effect on the natural history of the aneurysm.
Key Findings: Reductions in Rupture and Mortality
The results of the analysis were striking. After propensity score matching, which created two balanced cohorts of 2,275 patients each, the use of GLP-1RAs was found to be a significant protective factor.
Subarachnoid Hemorrhage Risk
Patients treated with GLP-1RAs experienced a significantly lower rate of nontraumatic subarachnoid hemorrhage compared to the control group. The calculated Hazard Ratio (HR) was 0.66 (95% CI, 0.50–0.87), representing a 34% reduction in the risk of rupture. This finding suggests that GLP-1RAs may play a role in stabilizing the aneurysm wall, potentially through the mitigation of chronic vascular inflammation.
All-Cause Mortality
The benefits of GLP-1RA therapy extended to overall survival. The treatment group showed a 37% lower risk of all-cause mortality (HR, 0.63 [95% CI, 0.52–0.76]). While this mortality benefit likely reflects the broad cardiovascular and metabolic advantages of GLP-1RAs, it underscores the safety and utility of these agents in patients with complex vascular comorbidities.
Untreated Aneurysm Subgroup
In the analysis focusing exclusively on patients whose aneurysms had not been surgically or endovascularly treated, the protective association remained robust. For these patients, GLP-1RA use was associated with an HR of 0.68 (95% CI, 0.47–0.98) for SAH and an HR of 0.64 (95% CI, 0.53–0.77) for all-cause mortality. This is particularly relevant for the large population of patients who are currently managed with “watchful waiting,” as it suggests a potential medical intervention to reduce their risk during observation.
Mechanistic Insights: Why GLP-1RAs Might Stabilize Aneurysms
The biological plausibility of these findings rests on the known expression of GLP-1 receptors in the brain and the vascular endothelium. Aneurysm rupture is often the culmination of a cycle of inflammation, oxidative stress, and matrix metalloproteinase (MMP) activity that weakens the vessel wall. GLP-1RAs have been shown in preclinical models to downregulate pro-inflammatory cytokines such as TNF-alpha and IL-6 and to inhibit the recruitment of macrophages to the vascular wall.
Furthermore, GLP-1RAs improve nitric oxide bioavailability and promote endothelial cell repair. By reducing systemic inflammation and potentially local vessel wall inflammation, these agents may help maintain the structural integrity of the aneurysm. Additionally, the mild blood-pressure-lowering effect of GLP-1RAs may contribute to reduced wall tension, although the PSM analysis controlled for hypertension, suggesting that the protective effect goes beyond mere pressure control.
Expert Commentary and Clinical Implications
The findings by Feghali et al. represent a potential paradigm shift in the medical management of intracranial aneurysms. For decades, clinicians have had few tools to offer patients with small or difficult-to-treat aneurysms beyond lifestyle modifications and smoking cessation. If these results are validated in prospective clinical trials, GLP-1RAs could become a first-line medical therapy for diabetic patients with incidental aneurysms.
However, experts caution that while the study is large and utilizes advanced statistical matching, its retrospective nature means that it can only establish association, not causation. The use of the TriNetX database, while powerful, is dependent on the accuracy of diagnostic coding and does not provide detailed information on aneurysm size, morphology, or location—all of which are critical determinants of rupture risk.
Clinicians should also consider that these findings specifically apply to patients with type 2 diabetes. Whether these benefits extend to non-diabetic individuals with IAs remains an open question that requires further investigation. Nevertheless, the falsification analysis performed by the authors—which showed no difference in the rate of unrelated medical encounters (like dermatology visits)—strengthens the argument that the observed benefit is a direct result of the medication rather than a bias related to better healthcare access.
Conclusion
This study provides compelling evidence that GLP-1 receptor agonists are associated with a significantly reduced risk of subarachnoid hemorrhage and improved survival in patients with intracranial aneurysms and type 2 diabetes. These findings highlight a promising new frontier in the pharmacological management of vascular disease. Given the high stakes of aneurysm rupture, prospective randomized controlled trials are urgently warranted to determine if GLP-1RAs should be formally integrated into the standard of care for patients with unruptured intracranial aneurysms.
References
1. Feghali J, Ruchika F, Horowitz MA, et al. Glucagon-Like Peptide-1 Receptor Agonists and Decreased Subarachnoid Hemorrhage Risk in Patients With Intracranial Aneurysm. Stroke. 2026;57(1). doi:10.1161/STROKEAHA.125.053599.
2. Thompson BG, Brown RD Jr, Amin-Hanjani S, et al. Guidelines for the Management of Patients With Unruptured Intracranial Aneurysms: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2015;46(8):2368-2400.
3. Drucker DJ. Mechanisms of Action and Therapeutic Application of Glucagon-like Peptide-1. Cell Metabolism. 2018;27(4):740-756.