Introduction: The Dilemma of Measuring Progression in Geographic Atrophy
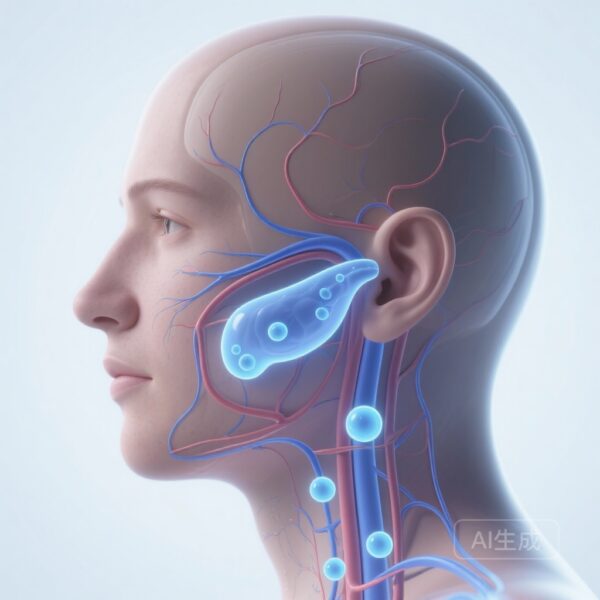
Geographic atrophy (GA), the advanced form of dry age-related macular degeneration (AMD), remains one of the most significant causes of irreversible vision loss worldwide. Characterized by the progressive loss of photoreceptors, retinal pigment epithelium (RPE), and choriocapillaris, GA results in expanding scotomas that eventually threaten central vision. In the current era of emerging therapeutics—marked by the recent approvals of complement inhibitors such as pegcetacoplan and avacincaptad pegol—the precision with which we measure disease progression has never been more critical.
Historically, clinical trials and longitudinal monitoring have relied on two primary endpoints: best-corrected visual acuity (BCVA) and GA lesion area. However, both measures possess inherent flaws. BCVA, while highly relevant to patient quality of life and recognized by regulatory bodies like the FDA, is notoriously subjective and prone to high test-retest variability. Conversely, the total GA area, measured via fundus autofluorescence (FAF) or color fundus photography (CFP), is objective and reproducible but suffers from a lack of functional nuance. It treats every square millimeter of the macula as having equal weight, failing to account for the disproportionate impact of foveal versus extrafoveal lesions on a patient’s functional vision.
To address this gap, a landmark study published in JAMA Ophthalmology has proposed and validated a novel metric: the Geographic Atrophy Weighted-by-Acuity Index (GAWAIN). This structural measure is designed to align with functional outcomes by empirically weighting macular locations based on their contribution to visual acuity.
Methodology: Deriving the GAWAIN Index
The Conceptual Framework
The core innovation of GAWAIN lies in its move away from simple area summation. The researchers hypothesized that by dividing the macula into concentric zones (annuli) and assigning a weight to each zone based on its correlation with visual deficit, they could create a structural surrogate that more accurately reflects functional decline. This approach acknowledges the physiological reality that the density of cones and the complexity of neural processing are highest in the fovea and decrease with eccentricity.
Study Design and Training Set
This prognostic study utilized a robust dataset for derivation and internal validation. The training set was derived from the Age-Related Eye Disease Study 2 (AREDS2), involving 1,528 eyes across 4,313 visits. The mean age of the training participants was 77.1 years, with a representative gender distribution (57.6% female).
The researchers divided the macula into 60 concentric annuli. For each visit, the GA occupancy (the percentage of the area covered by atrophy) within each annulus was calculated. Using ridge regression, the team identified the specific weight for each annulus, with GA involvement and age serving as predictors and the BCVA deficit (defined as 100 minus the BCVA letter score) as the primary outcome. The resulting weights demonstrated a decelerating decline as one moved from the foveal center toward the macular periphery, mirroring the known distribution of visual sensitivity.
External Validation
To ensure the generalizability of the index, the researchers applied the GAWAIN weights to an external validation set: the GA Minocycline Trial. This cohort included 35 participants (218 visits) with a mean age of 74.3 years. This step was crucial to demonstrate that the index remained effective across different clinical trial settings and imaging modalities, specifically color fundus photography (CFP) and fundus autofluorescence (FAF).
Key Findings: Superior Performance of GAWAIN
Cross-sectional Correlation with Function
The internal validation results were striking. GAWAIN demonstrated a significantly stronger correlation with BCVA deficit than traditional GA area measurements. The Pearson correlation coefficient (r) for GAWAIN was 0.58, compared to only 0.32 for the standard GA area (difference = 0.27; 95% CI, 0.23-0.31; P < .001). This suggests that GAWAIN captures nearly double the variance in visual acuity explained by structural atrophy compared to simple area metrics.
The superiority of GAWAIN held true in the external validation cohort as well. When using CFP-defined GA, the correlation was 0.69 for GAWAIN versus 0.58 for GA area. Using FAF-defined GA, the correlation was 0.70 for GAWAIN versus 0.56 for GA area. These results confirm that the weighting system is robust and not dependent on a specific imaging technique.
Predictive Accuracy for Clinical Thresholds
Clinicians often categorize vision loss based on functional thresholds, such as 20/20 (85 letters), 20/40 (70 letters), and 20/200 (35 letters). The study found that GAWAIN was significantly more accurate than GA area in predicting whether a patient’s vision had fallen below these critical marks (P < .001 for all thresholds). This predictive capability is vital for identifying patients at high risk of losing driving vision or legal blindness.
Longitudinal Sensitivity
Perhaps most importantly for clinical trialists, the change in GAWAIN over time correlated more strongly with the decline in BCVA than the change in total GA area did. In the internal validation cohort, the Pearson r for longitudinal change was 0.37 for GAWAIN compared to 0.28 for GA area (difference = 0.09; 95% CI, 0.04-0.14; P < .001). This indicates that GAWAIN is a more sensitive indicator of functional deterioration over the course of disease progression.
Clinical and Scientific Implications
Refining Clinical Trial Endpoints
The primary hurdle in GA drug development has been the “structure-function mismatch.” Many therapies have succeeded in slowing the growth of GA lesions (structure) but failed to show a concurrent benefit in visual acuity (function) within the typical two-year trial timeframe. This mismatch complicates regulatory approval and leaves clinicians questioning the real-world benefit of treatments.
GAWAIN offers a potential solution. By providing a structural measure that is mathematically aligned with functional loss, it may serve as a more meaningful surrogate endpoint. If a drug slows the progression of the GAWAIN index, it is inherently slowing a structural change that is more closely linked to how a patient actually sees, potentially providing a clearer path for regulatory appraisal.
Personalized Patient Management
In clinical practice, GAWAIN could improve the way we communicate risk to patients. Rather than telling a patient their lesion grew by 1.5 mm², a clinician could use a weighted index to explain how the expansion is encroaching on high-value retinal real estate. This could help in setting expectations for future vision loss and timing interventions more effectively.
Expert Commentary and Limitations
The development of GAWAIN represents a significant step toward the “holy grail” of retinal imaging: a structural biomarker that perfectly mirrors functional status. However, several considerations remain. First, while the correlation of 0.58 to 0.70 is a vast improvement over 0.32, it is not a perfect 1.0. This gap suggests that factors beyond RPE atrophy—such as photoreceptor health in non-atrophic areas, the presence of reticular pseudodrusen, or neuroplasticity in the visual cortex—also play a role in BCVA.
Additionally, while ridge regression and concentric annuli are mathematically sound, they assume a radial symmetry in the macula that may not exist for all patients. The impact of a lesion may vary not just by eccentricity but also by quadrant (e.g., superior vs. inferior), which this model does not currently distinguish. Furthermore, GAWAIN focuses on BCVA; future iterations might benefit from incorporating other functional measures such as microperimetry or low-luminance visual acuity, which are often more sensitive in early GA stages.
Conclusion
The Geographic Atrophy Weighted-by-Acuity Index (GAWAIN) marks a paradigm shift in how we quantify dry AMD progression. By integrating the topographical importance of the macula into a structural measurement, the authors have created a tool that is objective, reproducible, and functionally relevant. As the field moves toward more personalized and effective treatments for GA, metrics like GAWAIN will be indispensable in ensuring that structural successes in the lab translate into meaningful functional preservation for patients.
References
- Hou J, von der Emde L, Mukherjee S, et al.; AREDS2 Research Group. Proposal, Derivation, and External Validation of a Novel Geographic Atrophy Outcome Measure. JAMA Ophthalmol. Published online January 29, 2026. doi:10.1001/jamaophthalmol.2025.6002
- Chew EY, et al. Secondary analyses of the effects of lutein/zeaxanthin on age-related macular degeneration progression: AREDS2 report No. 3. JAMA Ophthalmol. 2014.
- Fleckenstein M, et al. The Progression of Geographic Atrophy Secondary to Age-Related Macular Degeneration. Ophthalmology. 2018.