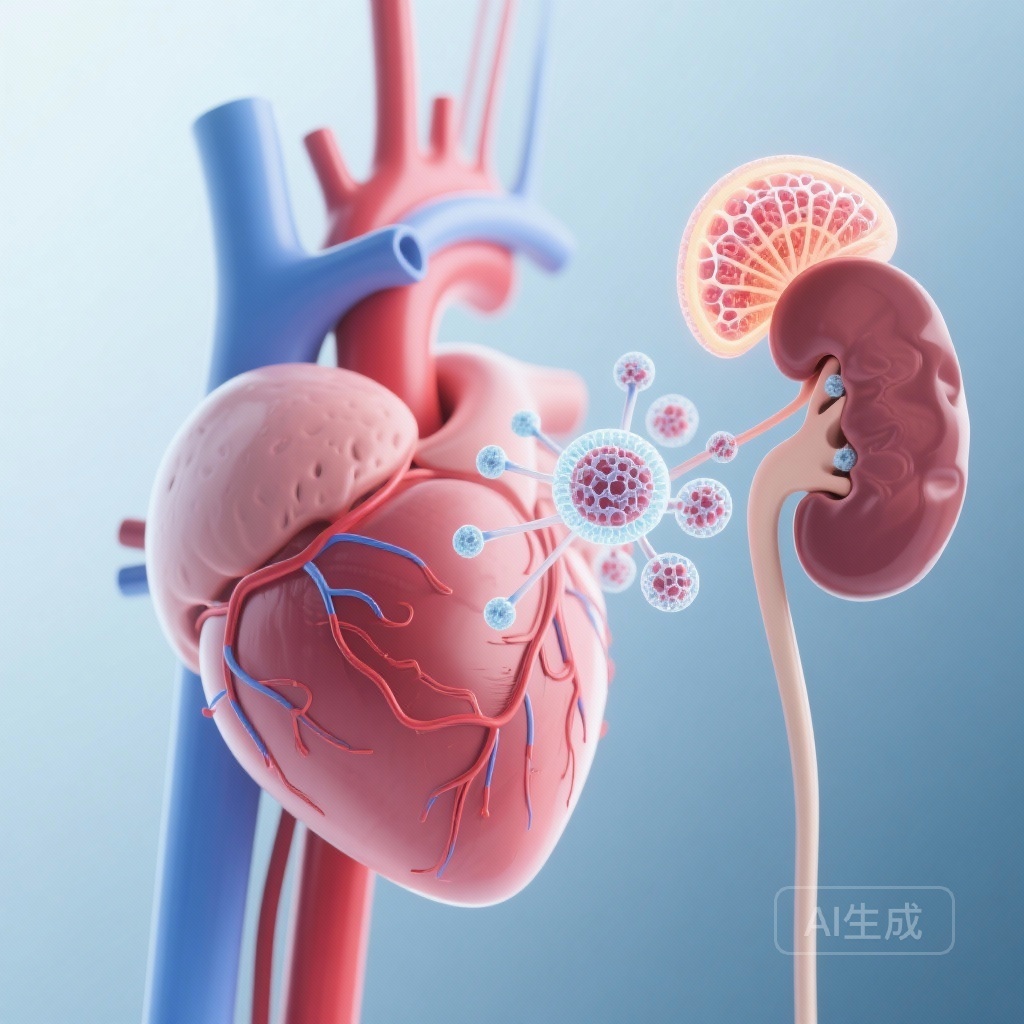
The Intertwined Pathophysiology of Heart and Kidney
The clinical management of heart failure (HF) is inextricably linked to renal function. In patients with heart failure with mildly reduced ejection fraction (HFmrEF) or preserved ejection fraction (HFpEF), the presence of chronic kidney disease (CKD) significantly complicates the therapeutic landscape and worsens prognosis. Traditionally, clinicians have relied on the estimated glomerular filtration rate (eGFR) to assess renal health, but contemporary evidence emphasizes that urine albumin-to-creatinine ratio (UACR) provides a complementary and equally vital dimension of kidney risk. The FINEARTS-HF trial, which investigated the non-steroidal mineralocorticoid receptor antagonist (MRA) finerenone, has provided a landmark dataset for understanding how these cardiorenal therapies perform across the spectrum of kidney health.
Highlights of the FINEARTS-HF Kidney Risk Analysis
1. Finerenone demonstrated consistent efficacy in reducing the primary endpoint of cardiovascular death and total heart failure events across all baseline KDIGO kidney risk categories (low, moderate, and high/very high).
2. Patients at higher baseline kidney risk experienced the most significant reductions in albuminuria after six months of treatment, suggesting a potent renoprotective effect where it is needed most.
3. The safety profile of finerenone, particularly regarding the risk of hyperkalemia, remained stable across kidney risk groups, provided that the baseline eGFR was above 25 mL/min/1.73 m2.
4. Health status improvements, measured by the Kansas City Cardiomyopathy Questionnaire (KCCQ), were consistently observed regardless of the patient’s renal status at the start of the trial.
Study Design and Methodology
The FINEARTS-HF trial (Finerenone Trial to Investigate Efficacy and Safety Superior to Placebo in Patients with Heart Failure) was a double-blind, randomized controlled trial. This specific prespecified analysis categorized 5,797 participants (97% of the total trial population) based on their baseline KDIGO (Kidney Disease: Improving Global Outcomes) risk classification. This classification is a robust tool that combines both eGFR and UACR to stratify patients into low, moderately increased, and high or very high kidney risk.
Participants were randomized to receive finerenone or a placebo. Key inclusion criteria required an eGFR of at least 25 mL/min/1.73 m2 and a serum potassium level of no more than 5.0 mmol/L. The primary endpoint was a composite of cardiovascular (CV) death and total (first and recurrent) HF events. Secondary endpoints included changes in the KCCQ Total Symptom Score, eGFR slope, and a composite kidney outcome.
Analysis of Key Findings
Consistency of Clinical Efficacy
At baseline, the distribution of kidney risk among participants was relatively even: 35% were low risk, 29% were moderate risk, and 36% were high or very high risk. Over a median follow-up of 2.7 years, the study confirmed that higher baseline kidney risk was a potent predictor of adverse outcomes. Patients in the high/very high risk KDIGO category had substantially higher rates of primary outcome events compared to those in the low-risk category.
Crucially, the treatment effect of finerenone was not attenuated by kidney risk. The reduction in CV death and total HF events was consistent across the groups (P-interaction = 0.24). This finding is particularly relevant for clinicians who may be hesitant to initiate MRA therapy in patients with advanced CKD due to fears of efficacy loss or complications.
Renoprotection and Albuminuria
One of the most striking results was the effect of finerenone on albuminuria. Participants with the highest baseline kidney risk saw the greatest relative reductions in UACR after 6 months of treatment (P-interaction = 0.031). While the eGFR slope (the rate of decline in kidney function over time) did not show a significant difference between treatment arms in this specific analysis, the reduction in albuminuria is a well-recognized surrogate for long-term renal preservation. This suggests that finerenone may modify the underlying disease process in the kidneys even as it stabilizes heart failure.
Patient-Reported Outcomes
Quality of life is a paramount concern in HFpEF and HFmrEF management. The KCCQ-Total Symptom Score at 12 months showed that finerenone improved symptoms and physical limitations consistently across all KDIGO categories (P-interaction = 0.36). This reinforces the role of finerenone as a therapy that not only prevents hard clinical endpoints but also helps patients feel better in their daily lives.
Safety and Tolerability in High-Risk Populations
Hyperkalemia is the primary safety concern associated with MRAs. In this analysis, the risk of safety events, including clinically significant hyperkalemia, was not disproportionately enhanced in patients with higher baseline kidney risk. While patients with lower eGFR and higher UACR are generally more prone to electrolyte imbalances, the protocol-driven monitoring and the pharmacological profile of finerenone—a non-steroidal MRA with a shorter half-life and balanced distribution between heart and kidney compared to spironolactone—contributed to a manageable safety profile.
Expert Commentary and Clinical Implications
The results of the FINEARTS-HF kidney risk analysis suggest that we must move beyond a ‘renal-centric’ fear of MRAs. For many years, patients with significant kidney impairment were excluded from trials or undertreated in clinical practice. Finerenone appears to bridge this gap, offering a therapeutic option that is safe and effective down to an eGFR of 25 mL/min/1.73 m2.
The biological plausibility of these findings lies in the overactivation of the mineralocorticoid receptor, which drives inflammation and fibrosis in both the heart and the kidneys. By providing a more targeted blockade, finerenone addresses the common pathways of cardiorenal syndrome. Clinicians should be encouraged to screen both eGFR and UACR in their heart failure patients to accurately assess risk and initiate therapy appropriately.
Conclusion
The FINEARTS-HF trial demonstrates that finerenone is a versatile and robust therapy for patients with HFmrEF and HFpEF across the entire spectrum of kidney risk. By improving clinical outcomes, reducing albuminuria, and enhancing health status without introducing prohibitive safety risks, finerenone establishes itself as a foundational component of cardiorenal care. Future research should continue to explore the long-term renal outcomes and the potential benefits of initiating such therapies even earlier in the disease course.
Funding and Clinical Trial Information
The FINEARTS-HF trial was funded by Bayer AG. ClinicalTrials.gov Identifier: NCT04435626.
References
Ostrominski JW, Mc Causland FR, Claggett BL, et al. Finerenone Across the Spectrum of Kidney Risk in Heart Failure: The FINEARTS-HF Trial. JACC Heart Fail. 2026;14(1):102439. doi: 10.1016/j.jchf.2025.03.006.