Highlights
Efficacy and Safety
Continuous erector spinae plane (ESP) block demonstrated non-inferior analgesic efficacy compared to conventional opioid-based regimens for patients undergoing video-assisted thoracoscopic lung resection (VATS).
Recovery Quality
Patients receiving the ESP block reported significantly higher Quality of Recovery-15 (QoR-15) scores at both 24 and 48 hours postoperatively, indicating a smoother transition and better overall well-being.
Clinical Outcomes
The ESP group experienced a significantly lower incidence of postoperative pulmonary complications (PPCs) and typical opioid-related side effects such as nausea, retching, and dizziness.
Background
Video-assisted thoracoscopic surgery (VATS) has revolutionized thoracic oncology and pulmonary medicine by reducing surgical trauma and shortening hospital stays. However, despite its minimally invasive nature, VATS is associated with significant acute postoperative pain. This pain stems from intercostal nerve irritation, rib spreading (in some cases), and the presence of chest tubes, which can impede deep breathing and coughing, ultimately increasing the risk of pulmonary complications.
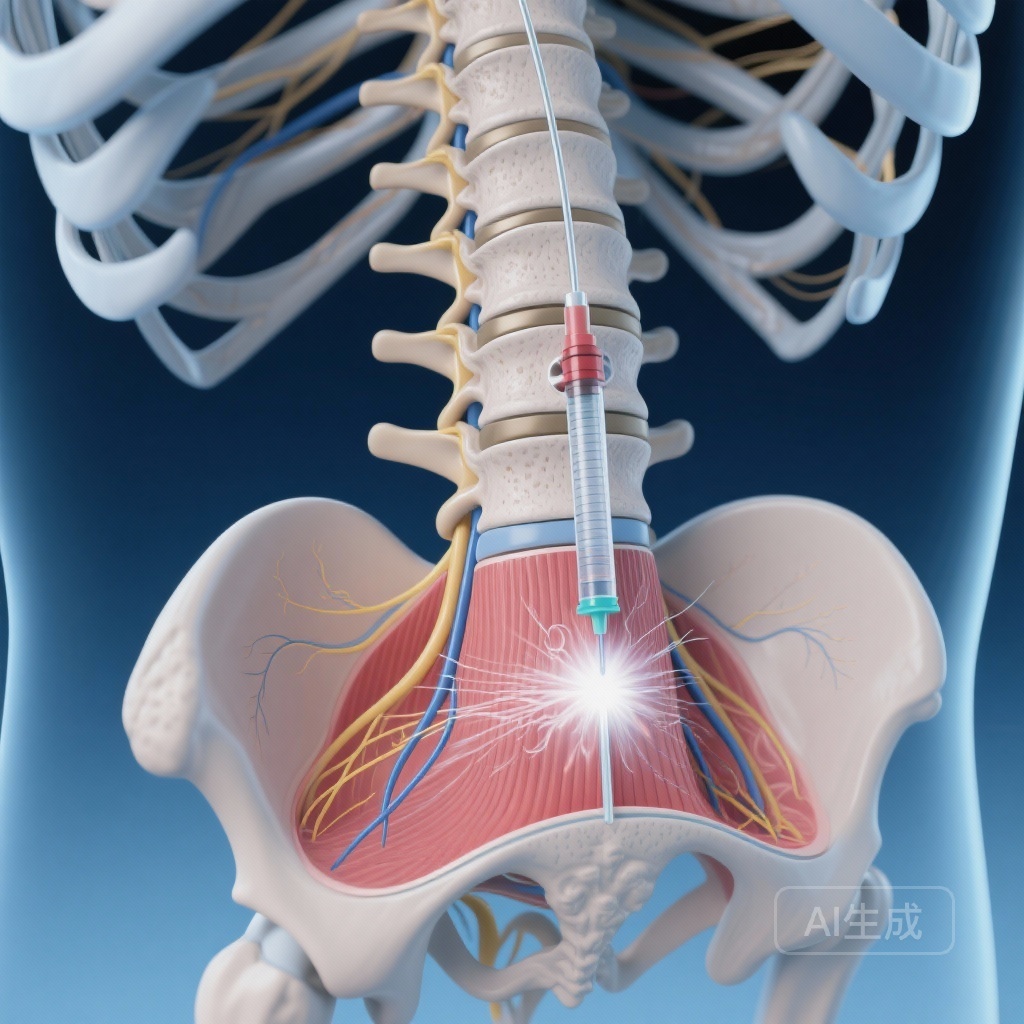
Traditionally, systemic opioids have been the cornerstone of postoperative analgesia. While effective, opioids are associated with a well-documented profile of adverse effects, including respiratory depression, nausea, vomiting, and ileus, which can delay recovery. Consequently, there is a clinical imperative to develop opioid-sparing multimodal analgesic strategies. Regional anesthesia, particularly fascial plane blocks like the erector spinae plane (ESP) block, has emerged as a promising alternative. The ESP block involves injecting local anesthetic into the fascial plane between the erector spinae muscle and the thoracic transverse processes, targeting the dorsal and ventral rami of the spinal nerves. While single-injection ESP blocks are common, this trial investigated the efficacy of continuous ESP block compared to standard opioid infusions.
Study Design
This was a prospective, randomized, open-label, non-inferiority trial conducted to compare continuous ESP block with a conventional opioid-based regimen in patients undergoing VATS lung resection. The trial sought to determine if the ESP block could provide equivalent pain control while offering superior recovery profiles.
Patient Allocation and Interventions
Patients were randomly assigned to one of two groups:
1. Continuous ESP Block Group: Patients received a continuous infusion of 0.25% ropivacaine via perineural catheters at a rate of 5 ml per hour. This was supplemented by a programmed intermittent bolus (PIB) of 10 ml every 6 hours for the initial 24 hours.
2. Conventional Opioid Group: Patients received a continuous infusion of sufentanil (2 μg/kg) and ondansetron (16 mg) diluted to 100 ml, administered at 2 ml per hour for 48 hours.
Endpoints
The primary outcome was the cumulative area under the curve (AUC) for the pain numeric rating scale (NRS) scores during coughing, measured from the time of discharge from the post-anaesthesia care unit (PACU) to 48 hours postoperatively. Secondary outcomes included the Quality of Recovery-15 (QoR-15) scores, the incidence of postoperative pulmonary complications (PPCs), and the frequency of adverse events like nausea, vomiting, and dizziness.
Key Findings
The results of the trial provide robust evidence supporting the use of continuous ESP blocks in thoracic surgery.
Primary Analgesic Efficacy
The study met its primary endpoint for non-inferiority. The cumulative AUC for pain NRS scores during coughing in the ESP block group was comparable to the opioid group. The mean difference was -0.99 (95% CI -11.97 to 9.98, p = 0.011 for non-inferiority). This suggests that the regional technique is just as effective as systemic opioids in managing the dynamic pain associated with coughing and movement after lung surgery.
Quality of Recovery and Pulmonary Function
One of the most striking findings was the difference in recovery quality. The ESP block group showed significantly superior QoR-15 scores at 24 hours (median difference 11, 95% CI 6–16, p < 0.001) and 48 hours (median difference 10, 95% CI 7–15, p < 0.001). Furthermore, the ESP group had a reduced risk of postoperative pulmonary complications (Relative Risk 0.45, 95% CI 0.21–0.96, p = 0.031). This is likely due to the superior pain control during coughing, which allows for better pulmonary toilet and atelectasis prevention.
Safety and Side Effects
The safety profile strongly favored the regional anesthesia approach. Patients in the ESP block group experienced significantly lower incidences of:
– Postoperative nausea (RR 0.17, p = 0.005)
– Retching (RR 0.11, p = 0.023)
– Dizziness (RR 0.22, p = 0.005)
These findings highlight the benefit of avoiding high-dose systemic opioids, which are the primary drivers of these distressing symptoms.
Expert Commentary
The success of the continuous ESP block in this trial underscores a broader shift in perioperative medicine toward Enhanced Recovery After Surgery (ERAS) protocols. By utilizing a fascial plane block, clinicians can achieve effective dermatomal coverage while minimizing the systemic burden of opioids. The use of programmed intermittent bolus (PIB) in this study is particularly noteworthy; emerging evidence suggests that intermittent boluses may provide better anesthetic spread within the fascial plane compared to a simple continuous infusion, potentially explaining the high efficacy observed.
However, it is important to note the open-label design of the study, which could introduce bias in subjective recovery reporting. Additionally, while the ESP block is technically simpler than thoracic epidural anesthesia—often considered the gold standard—it requires ultrasound expertise and careful catheter placement to ensure consistent results. Clinicians should also consider the resource requirements for maintaining continuous peripheral nerve blocks on the ward compared to standard intravenous infusions.
Conclusion
Following video-assisted thoracoscopic lung resection, continuous erector spinae plane block provides non-inferior postoperative analgesia when compared with conventional opioid-based regimens. More importantly, it significantly enhances the quality of patient recovery and reduces the risk of postoperative pulmonary complications and opioid-related side effects. These findings suggest that continuous ESP block should be considered a primary analgesic modality in the multimodal management of patients undergoing VATS.
References
Hu J, Zhou W, Zheng X, Zhang A, Huang Q, Zhang C, Yao Y, Lu D, Wei W. Analgesic efficacy of continuous erector spinae plane block vs. opioid-based regimen for postoperative pain management following video-assisted thoracoscopic lung resection: a prospective, randomised, open-label, non-inferiority trial. Anaesthesia. 2025 Oct;80(10):1226-1236. doi: 10.1111/anae.16651. Epub 2025 Jun 23. PMID: 40545885.