Highlights
Durable Functional Independence
At the three-year mark, patients treated with endovascular thrombectomy (EVT) for acute basilar artery occlusion (BAO) were twice as likely to achieve functional independence (mRS 0-3) compared to those receiving best medical management alone.
Significant Mortality Reduction
EVT demonstrated a sustained survival benefit, with a 3-year mortality rate of 55.7% compared to 73.1% in the medical management group, representing a clinically significant reduction in long-term mortality for this catastrophic stroke subtype.
Age-Dependent Efficacy
While the overall cohort showed clear benefits, prespecified subgroup analyses indicated that the treatment effect was most pronounced in patients younger than 70 years, whereas patients aged 70 and older did not show a statistically significant treatment effect at the 3-year interval.
Background: The Challenge of Basilar Artery Occlusion
Acute basilar artery occlusion (BAO) represents one of the most devastating forms of ischemic stroke, historically associated with mortality rates exceeding 80% and severe neurological disability among survivors. The posterior circulation, which supplies the brainstem, cerebellum, and thalamus, is critical for life-sustaining functions, making rapid and effective recalculation essential.
While endovascular thrombectomy (EVT) has revolutionized the treatment of anterior circulation large vessel occlusions, its role in BAO remained a subject of intense debate for years due to the failure of early randomized trials to demonstrate superiority over medical management. However, recent landmark trials, including ATTENTION and BAOCHE, provided high-level evidence for the short-term (90-day) efficacy of EVT. Despite these successes, the long-term durability of these benefits remained an open question. Clinicians and policy makers needed to know whether the initial gains in functional recovery would persist or diminish over several years, especially given the high risk of recurrent vascular events and the frailty often associated with BAO survivors.
Study Design and Methodology
The 3-year follow-up of the ATTENTION (Endovascular Treatment of Acute Basilar Artery Occlusion) trial was designed to address this evidence gap. This multicenter, open-label, assessor-blinded randomized clinical trial was conducted across 36 comprehensive stroke centers in China.
Participant Selection
Between February 2021 and January 2022, the study enrolled 340 adult patients with imaging-confirmed acute BAO presenting within 12 hours of symptom onset. Patients were randomized in a 2:1 ratio to receive either EVT plus best medical management (n=226) or best medical management alone (n=114). The analysis for the 3-year extension included 307 patients (90.3% of the original cohort) who completed the full follow-up period through January 2025.
Interventions
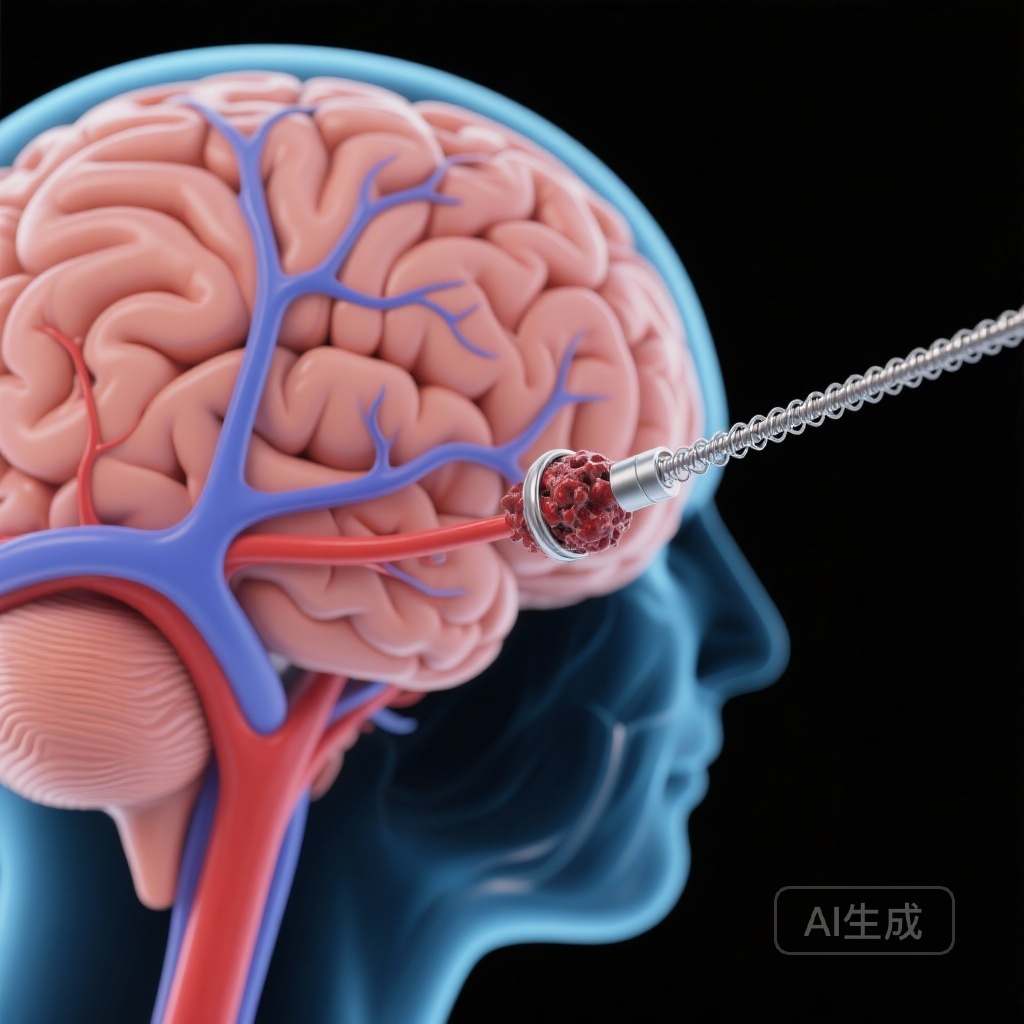
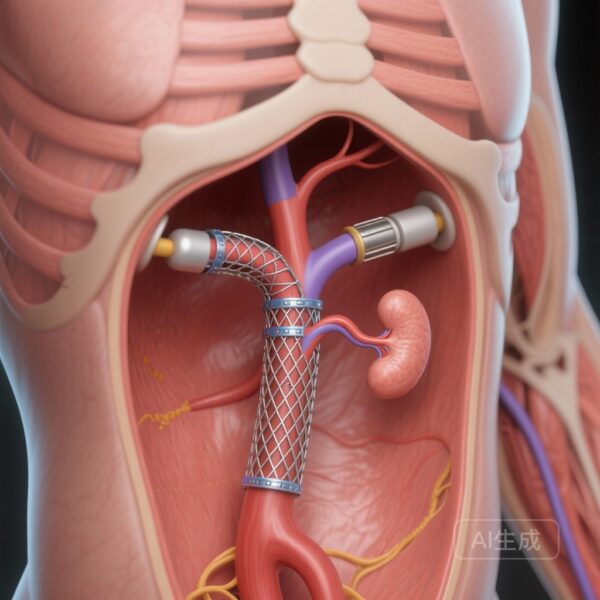
In the EVT group, the choice of endovascular technique—including stent retrievers, aspiration catheters, balloon angioplasty, or intra-arterial thrombolysis—was left to the discretion of the treating neuro-interventionalist. The control group received current standard-of-care medical therapy, which could include intravenous thrombolysis if within the appropriate time window, as well as antiplatelet or anticoagulant therapy.
Endpoints
The primary outcome for the long-term follow-up was functional independence, defined as a modified Rankin Scale (mRS) score of 0 to 3 at 3 years. Secondary outcomes included narrower definitions of recovery (mRS 0-2), the overall distribution of mRS scores (shift analysis), and cumulative mortality.
Key Findings: Long-Term Clinical Outcomes
The results of the 3-year follow-up provide robust evidence for the sustained benefit of mechanical intervention in BAO.
Primary Outcome: Functional Recovery
At 3 years, 38.4% (78 of 203) of patients in the thrombectomy group achieved an mRS score of 0 to 3, compared with only 18.3% (19 of 104) in the medical management group. After adjusting for baseline variables, the risk ratio (RR) for achieving this level of functional independence was 2.05 (95% CI, 1.35-3.11; P = .001). This indicates that patients receiving EVT were more than twice as likely to remain functional enough to walk and care for themselves three years after their stroke.
Secondary Outcomes and Shift Analysis
When examining the full range of neurological outcomes via the mRS shift analysis, the thrombectomy group showed a significant shift toward better outcomes (adjusted common odds ratio, 2.60; 95% CI, 1.53-4.43). The percentage of patients achieving excellent recovery (mRS 0-2) was also higher in the EVT group compared to the control group.
Mortality Data
Mortality in BAO remains high regardless of treatment, reflecting the severity of the initial insult. However, EVT significantly lowered the ceiling. Cumulative 3-year mortality was 55.7% in the EVT group compared to 73.1% in the medical management group (adjusted RR, 0.76; 95% CI, 0.65-0.89). Notably, mortality increased in both groups between the 90-day and 3-year marks, but the relative advantage of EVT was preserved over time.
Subgroup Analysis: The Age Factor
One of the most critical findings from the prespecified subgroup analysis involved patient age. The benefit of EVT was strikingly clear in patients under the age of 70. Conversely, in patients aged 70 years and older, the study did not demonstrate a statistically significant difference in 3-year functional outcomes between the two treatment arms. This suggests that while age alone should not be an absolute contraindication, clinicians must carefully consider baseline frailty and comorbidities in older populations when making treatment decisions.
Clinical Interpretation and Expert Commentary
The ATTENTION 3-year results represent a milestone in stroke neurology. They move the conversation beyond the acute phase of care, proving that the “salvage” of brainstem tissue during the first 12 hours of a stroke translates into years of improved quality of life and survival.
The durability of the treatment effect is particularly noteworthy. In many cardiovascular and neurological interventions, the benefit seen at 30 or 90 days can be diluted by long-term complications or secondary events. In the case of BAO, the initial successful recanalization appears to provide a “functional reserve” that helps patients withstand the challenges of aging and secondary vascular risks over the subsequent years.
However, the high mortality rate—even in the treatment group—cannot be ignored. With more than half of the EVT patients deceased by year three, BAO remains a high-stakes clinical emergency. These findings underscore the need not only for rapid intervention but also for aggressive secondary prevention and long-term neuro-rehabilitation to protect the gains made during the acute procedure.
Regarding the age-related findings, experts suggest that the lack of significant benefit in the elderly (70+) may be due to a higher burden of pre-existing small vessel disease, reduced neuroplasticity, or the competing risks of non-neurological mortality. Further research is needed to refine patient selection in the elderly to ensure that those most likely to benefit are identified.
Conclusion
The 3-year outcomes of the ATTENTION trial confirm that endovascular thrombectomy is a highly effective and durable intervention for acute basilar artery occlusion. By doubling the chances of functional independence and significantly reducing long-term mortality, EVT has solidified its position as the standard of care. These results provide a powerful mandate for healthcare systems to optimize stroke referral pathways, ensuring that patients with suspected posterior circulation strokes have rapid access to comprehensive stroke centers capable of performing mechanical thrombectomy.
Funding and Clinical Trial Registration
This study was supported by various regional and national health research funds in China. The trial is registered at ChiCTR.org.cn (Identifier: ChiCTR2400082236).
References
1. Hu W, Tao C, Li R, et al. Endovascular vs Medical Treatment of Basilar Artery Occlusion: 3-Year Outcomes of the ATTENTION Randomized Clinical Trial. JAMA Neurol. 2025; Published online December 29, 2024. doi:10.1001/jamaneurol.2025.5077.
2. Tao C, Nogueira RG, Zhu Y, et al; ATTENTION Investigators. Trial of Endovascular Treatment of Acute Basilar Artery Occlusion. N Engl J Med. 2022;387(15):1361-1372.
3. Jovin TG, Li C, Wu L, et al; BAOCHE Investigators. Trial of Thrombectomy 6 to 24 Hours after Stroke Due to Basilar-Artery Occlusion. N Engl J Med. 2022;387(15):1373-1384.
4. Ghozy S, Siegler JE, Tjoumakaris S, et al. Mechanical Thrombectomy in Basilar Artery Occlusion: A Systematic Review and Meta-analysis. JAMA Netw Open. 2022;5(11):e2243733.