Endoscopic Radial Artery Harvesting: Improving Functional Outcomes and Neurologic Safety in CABG
In the field of coronary artery bypass grafting (CABG), the selection of arterial conduits has a profound impact on long-term graft patency and patient survival. The radial artery (RA) is frequently utilized as a secondary conduit due to its superior patency rates compared to the long saphenous vein. However, the method of harvesting the radial artery remains a subject of clinical debate. While the traditional open radial artery harvest (ORAH) provides direct visualization, it is associated with significant donor-site morbidity, including scarring, pain, and neurologic impairment. The emergence of endoscopic radial artery harvest (ERAH) offered a minimally invasive alternative, yet high-level evidence comparing the two techniques—particularly regarding patient-reported functional outcomes—has been sparse until recently.
Highlight
ERAH significantly reduces the risk of post-operative neurologic deficits, with ORAH patients facing more than twice the risk of sensory or motor impairment. Patients undergoing the endoscopic approach reported modestly better hand function at three months, suggesting a faster and more complete return to baseline activities. Despite the complexity of the endoscopic technique, the trial demonstrated a safety profile comparable to the open approach, supporting its broader clinical adoption.
The Clinical Context of Radial Artery Harvesting
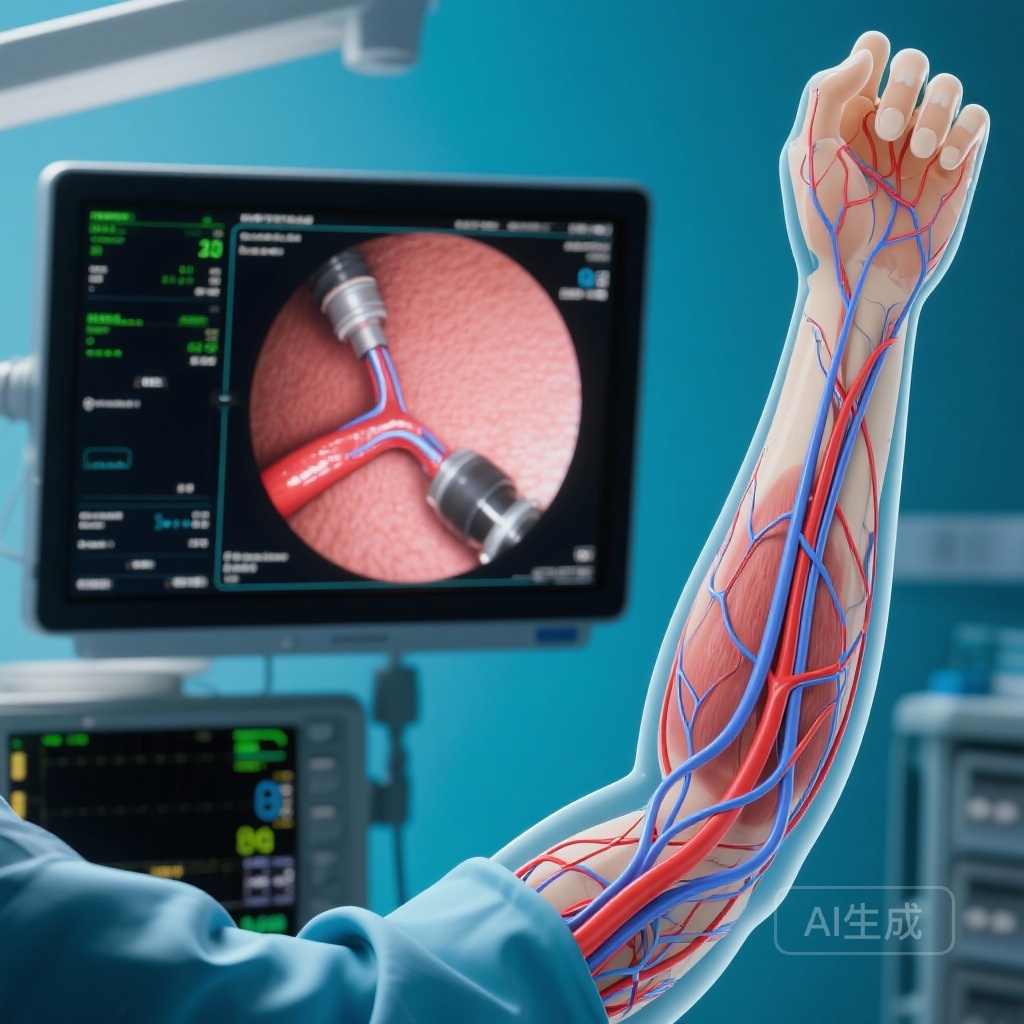
For decades, the radial artery has been harvested through a large longitudinal incision extending from the wrist to the antecubital fossa. While effective for obtaining a high-quality conduit, this ‘open’ approach leaves a prominent scar and exposes the superficial branch of the radial nerve and the lateral antebrachial cutaneous nerve to potential injury. Patients often complain of persistent numbness, paresthesia, and reduced grip strength, which can negatively affect their quality of life post-CABG.
ERAH was developed to mitigate these issues by utilizing small incisions and specialized endoscopic equipment to dissect the artery under video guidance. Despite its theoretical advantages, concerns regarding the learning curve, the potential for thermal injury to the graft, and the cost of the equipment have prevented it from becoming the universal standard. The study published in NEJM Evidence (Carranza et al., 2026) provides much-needed clarity on these competing priorities.
Study Design and Methodology
This randomized controlled trial (NCT01848886) enrolled 300 adult patients scheduled for CABG who required a radial artery graft. Participants were randomly assigned in a 1:1 ratio to either ERAH (n=151) or ORAH (n=149).
The primary endpoint was patient-reported hand function at three months post-randomization, measured using the Hand Function Questionnaire (HFQ). The HFQ scores range from 5 to 49, where lower scores represent better functionality. Secondary endpoints focused on objective neurologic deficits, including sensory loss or motor weakness in the distribution of the radial and cutaneous nerves. The researchers also monitored serious adverse events (SAEs) to ensure that the minimally invasive approach did not compromise patient safety.
Key Findings: Functional and Neurologic Outcomes
Hand Function Recovery
At the three-month follow-up, patients in the ERAH group reported superior hand function compared to those in the ORAH group. The mean HFQ score for ERAH patients was 7.20, while the ORAH group averaged 7.74. This resulted in a statistically significant difference of 0.52 points (95% CI, 0.06 to 0.98; P=0.03). While the magnitude of this difference did not reach the suggested minimal clinically important difference (MCID) of 3 points, it indicates a consistent trend toward better subjective recovery in the endoscopic cohort.
Neurologic Deficits: The Defining Advantage
The most striking finding of the trial was the disparity in neurologic complications. In the ORAH group, 82 out of 149 patients (55.0%) exhibited neurologic deficits at the three-month mark. In contrast, only 32 out of 151 patients (21.2%) in the ERAH group experienced similar issues. This represents a relative risk of 2.61 for neurologic deficits in the open harvest group (95% CI, 1.90 to 3.63), highlighting the protective effect of the endoscopic approach on peripheral nerve integrity.
Safety and Adverse Events
Safety data suggested that ERAH is a viable and safe alternative to open surgery. Serious adverse events occurred in 9 of 151 patients (6.0%) in the ERAH group, compared to 4 of 149 patients (2.7%) in the ORAH group. Although the raw percentage was slightly higher in the endoscopic group, the difference was not statistically significant (relative risk 0.45; 95% CI, 0.13 to 1.34). Most SAEs were related to general post-operative complications rather than the harvesting technique itself.
Expert Commentary: Clinical Implications and Limitations
The results of this trial suggest that ERAH should be the preferred method for radial artery acquisition in centers with the necessary expertise. The massive reduction in neurologic deficits—from over half of patients in the open group to roughly one-fifth in the endoscopic group—is a compelling argument for the minimally invasive approach.
However, clinicians must interpret the primary outcome with nuance. While the difference in HFQ scores was statistically significant, the absolute difference was small. This suggests that while patients feel ‘better’ with ERAH, the functional impact on daily living might be subtle for the average patient. The true value of ERAH may lie in the prevention of long-term neuropathic pain and the aesthetic benefit of avoiding a long forearm scar, which were not the primary focuses of this specific metric but are highly valued by patients.
One limitation of the study is the lack of long-term graft patency data. Critics of endoscopic harvesting often worry that the manipulation of the artery through a small tunnel could lead to endothelial damage or early graft failure. Future follow-up studies comparing the long-term survival and revascularization rates of ERAH vs. ORAH grafts will be essential to confirm that the short-term morbidity benefits do not come at the cost of long-term cardiac outcomes.
Conclusion
In patients undergoing coronary artery bypass surgery, endoscopic radial artery harvest offers clear advantages over the traditional open technique. By significantly reducing the incidence of neurologic deficits and providing a modest improvement in patient-reported hand function, ERAH addresses the primary morbidity concerns associated with radial artery conduits. As surgical teams continue to prioritize patient-centered outcomes and minimally invasive techniques, ERAH is likely to become the gold standard for arterial graft harvesting in modern cardiac surgery.
Funding and Clinical Trial Information
This study was registered at ClinicalTrials.gov under the identifier NCT01848886. The research was supported by institutional grants and focused on improving surgical standards for revascularization procedures.
References
1. Carranza CL, Petersen JJ, Ballegaard M, et al. Endoscopic or Open Radial Artery Harvest in Coronary Artery Bypass Surgery. NEJM Evid. 2026;5(1):EVIDoa2500199. doi:10.1056/EVIDoa2500199.
2. Gaudino M, Taggart D, Suma H, Puskas JD, Bhatt DL, Fremes SE. The Radial Artery for Coronary Artery Bypass Grafting: A Systematic Review and Meta-Analysis. JAMA Cardiol. 2020.
3. Ferdinand FD, MacDonald JK, Balkhy HH, et al. Endoscopic Radial Artery Harvesting: A Meta-Analysis of Outcomes. Innovations (Phila). 2017.