Introduction: The Clinical Paradox of SGLT2 Inhibition
Sodium-glucose cotransporter 2 (SGLT2) inhibitors have redefined the therapeutic landscape for type 2 diabetes (T2D), providing significant cardiorenal protection and glycemic efficacy. However, their primary mechanism—the induction of therapeutic glycosuria—creates an environment in the urinary tract that may favor the growth of urogenital pathogens. Clinical experience has long noted a higher incidence of mycotic and bacterial infections in patients on SGLT2 inhibitors, which frequently leads to reduced compliance and treatment discontinuation. Interestingly, emerging clinical data suggests that the concomitant use of dipeptidyl-peptidase four (DPP-4) inhibitors might mitigate these adverse effects. A recent study by Calvigioni et al. (2026) provides a microbiological basis for this observation, exploring how these agents, alone and in combination, modulate the resident urinary microbiota.
The Urinary Microbiome in Type 2 Diabetes: A State of Dysbiosis
Historically, the bladder was considered sterile; however, modern sequencing techniques have revealed a complex ‘urobiome’ that plays a critical role in mucosal health. In patients with T2D, this ecosystem is often disrupted. The study under review utilized 16S rRNA gene sequencing and quantitative PCR to establish a baseline for T2D patients compared to healthy controls.
At baseline, the researchers found that individuals with T2D exhibited a significantly higher total bacterial load and a distinct shift in microbial composition. Specifically, there was a higher abundance of the phylum Bacillota (formerly Firmicutes) compared to healthy individuals. This baseline dysbiosis suggests that the metabolic derangements of diabetes already predispose the urinary tract to an altered microbial environment, which may be further exacerbated by pharmacological interventions.
Study Design and Methodology
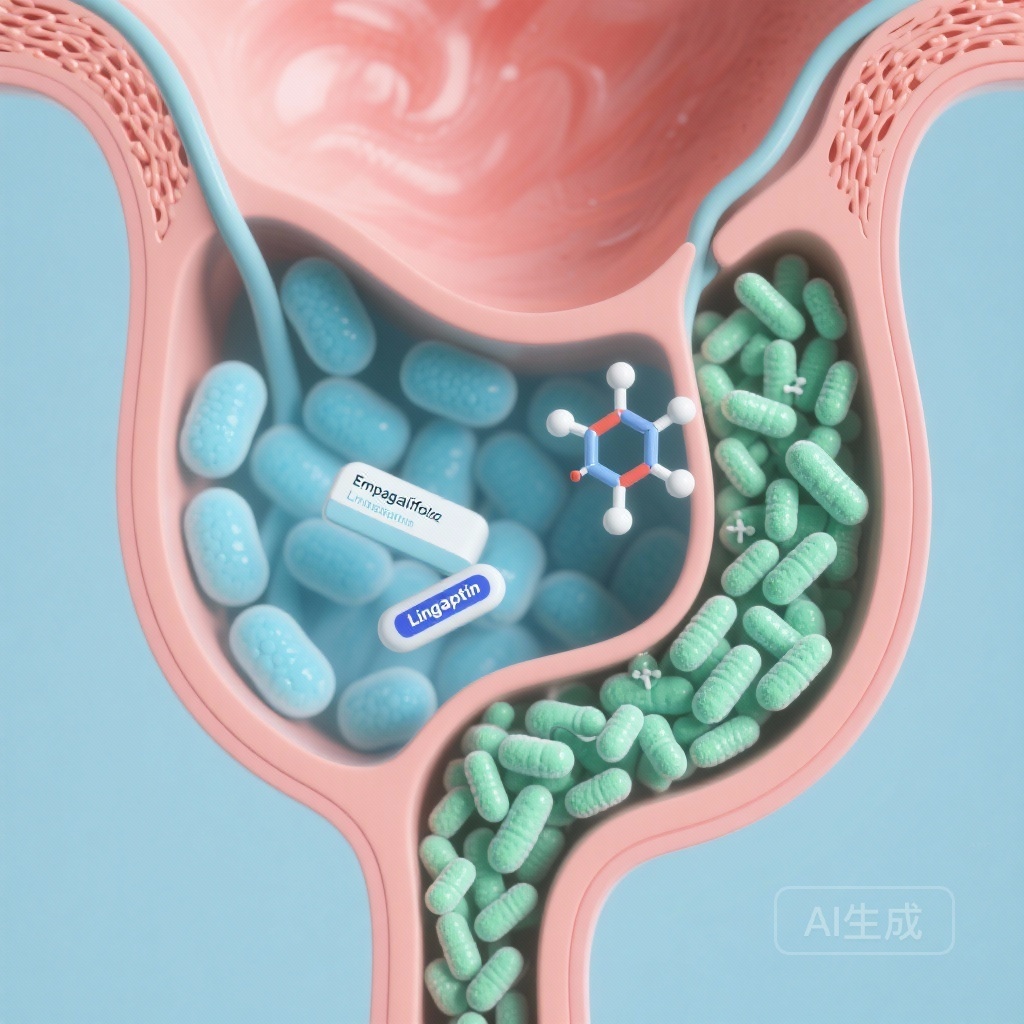
To investigate the impact of pharmacotherapy, an open-label, randomized clinical study was conducted on 30 individuals with T2D over a 12-week period. Participants were randomized to receive either Empagliflozin monotherapy or a combination of Empagliflozin and Linagliptin. A cohort of 15 healthy individuals served as the baseline control group. The researchers monitored clinical parameters, including BMI, fasting glucose, and HbA1c, alongside a rigorous evaluation of the urinary microbiota through Real-Time quantitative PCR and 16S rRNA gene sequencing.
Results: Differential Effects of Mono and Combination Therapy
The findings revealed a stark contrast between the two treatment arms, both in clinical outcomes and microbiological shifts.
Clinical Parameters
Both treatment groups saw a reduction in BMI over the 12-week period. However, the combination therapy (Empagliflozin/Linagliptin) was significantly more effective in improving glycemic markers. While fasting glucose and HbA1c levels improved in the combination arm, the improvements in the Empagliflozin monotherapy group did not reach the same level of statistical significance within the study timeframe, highlighting the synergistic metabolic effect of the dual-mechanism approach.
Microbiological Shifts
The most striking results were found in the composition of the urinary microbiota. In the Empagliflozin monotherapy group, there was a measurable increase in the total bacterial load of Bacillota and a specific increase in the genus Aerococcus. Aerococcus species are increasingly recognized as opportunistic urinary pathogens, and their proliferation under SGLT2 inhibitor monotherapy may explain the increased clinical risk of urogenital infections.
Conversely, the combination of Empagliflozin and Linagliptin appeared to ‘rescue’ the urobiome. In these patients, the microbial community was restored to a state closely resembling that of the healthy controls. Furthermore, the combination therapy significantly reduced the prevalence of potential urinary pathogens compared to the monotherapy group. This suggests that the addition of a DPP-4 inhibitor counteracts the dysbiotic pressure exerted by glycosuria.
Expert Commentary: Mechanistic Insights and Clinical Utility
The observation that Linagliptin can normalize the urinary microbiota despite the presence of SGLT2i-induced glycosuria is clinically significant. While the study does not fully elucidate the molecular mechanism, several hypotheses exist. DPP-4 is expressed on the surface of various immune cells and the urogenital epithelium; its inhibition may modulate local inflammatory responses or alter the availability of signaling peptides that influence bacterial adhesion and growth.
From a clinical perspective, these findings are highly relevant for patient adherence. If combination therapy can reduce the incidence of urogenital side effects by maintaining a healthy urinary microbiota, it may improve the persistence of SGLT2 inhibitor therapy, allowing more patients to benefit from the long-term cardiovascular and renal advantages of the class. This study supports a more proactive use of combination therapy, particularly in patients with a history of recurrent urogenital infections or those with evidence of significant baseline dysbiosis.
Conclusion: A New Rational for Combination Therapy
The study by Calvigioni et al. demonstrates that urinary dysbiosis is a feature of T2D and that SGLT2 inhibitor monotherapy can potentially worsen this state by favoring the growth of opportunistic pathogens like Aerococcus. However, the combination of Empagliflozin and Linagliptin effectively restores microbial homeostasis. This research provides a microbiological rationale for the observed clinical benefits of combining SGLT2 and DPP-4 inhibitors, pointing toward a strategy that optimizes both metabolic control and treatment tolerability. Future large-scale studies should confirm whether these microbiological changes translate directly into a lower incidence of symptomatic urinary tract infections in real-world clinical practice.
References
Calvigioni M, Biancalana E, Rossi C, Mazzantini D, Celandroni F, Ghelardi E, Solini A. Effect of SGLT2 Inhibitors + DPP-4 Inhibitors on Urine Microbiota in Type 2 Diabetes. Diabetes Metab Res Rev. 2026 Jan;42(1):e70127. doi: 10.1002/dmrr.70127. PMID: 41566786.