Highlights
- Emergent carotid artery stenting (eCAS) is associated with a 47% higher likelihood of improved functional outcomes at one year compared to non-eCAS strategies.
- The recanalization rate was significantly higher in the eCAS group (OR 4.28), facilitating better clinical recovery.
- The safety profile of eCAS remains robust, with no significant increase in hemorrhagic transformation or mortality rates.
- Benefit was consistent across both moderate (50-69%) and severe (≥70%) carotid stenosis, suggesting a broader utility for acute stenting.
Introduction: The Clinical Conundrum of Tandem Lesions
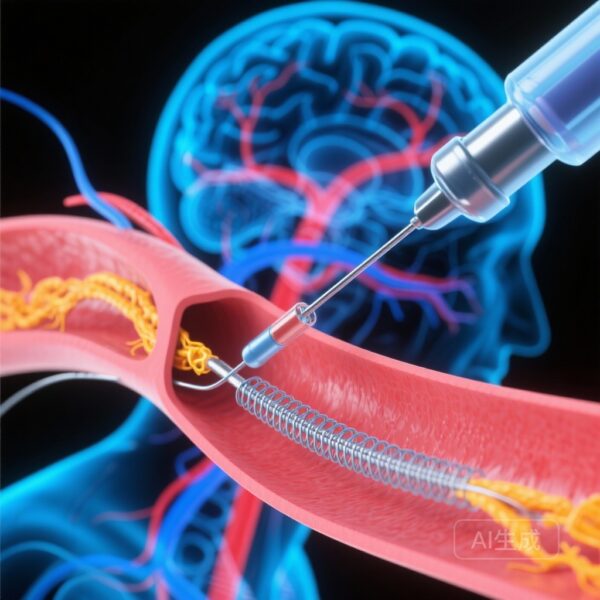
Tandem lesions (TL)—defined as the simultaneous occurrence of a high-grade cervical internal carotid artery (ICA) stenosis or occlusion and a distal intracranial large vessel occlusion (LVO)—represent approximately 15% to 25% of all acute ischemic strokes (AIS). These cases present a significant technical and clinical challenge for neurointerventionalists. While endovascular therapy (EVT) has become the gold standard for LVO, the optimal management of the proximal carotid lesion during the acute phase remains a subject of intense debate.
Clinicians must decide between a “carotid-first” or “thrombectomy-first” approach, and more critically, whether to perform emergent carotid artery stenting (eCAS) or rely on balloon angioplasty or medical management alone. Historically, concerns regarding the need for aggressive periprocedural antiplatelet therapy and the subsequent risk of intracranial hemorrhage (ICH) have tempered enthusiasm for eCAS. However, long-term data comparing these strategies have been lacking. The SECURIS study addresses this gap by providing one-year follow-up data from a large, prospective population-based registry.
Study Design and Methodology
The SECURIS study utilized data from the Code Stroke registry in Catalonia, Spain, a prospective mandatory population-based database. The researchers analyzed 578 patients treated between 2017 and 2023 who presented with AIS due to LVO and an ipsilateral atheromatous cervical ICA stenosis of at least 50%.
Participants were divided into two cohorts: those who received eCAS during the endovascular procedure (n=344) and those who did not (non-eCAS, n=234). The study employed inverse probability of treatment weighting (IPTW) to adjust for baseline imbalances and potential confounding factors, ensuring a more rigorous comparison between the two treatment arms.
The primary outcome was the shift in the modified Rankin Scale (mRS) score at 90 days and one year. Secondary outcomes included successful recanalization (defined as a modified Thrombolysis in Cerebral Infarction [mTICI] score of 2b or higher), favorable functional outcome (mRS 0-2), rates of hemorrhagic transformation (HT), and mortality. The researchers also conducted stratified analyses across age, sex, stenosis severity, and baseline NIH Stroke Scale (NIHSS) scores.
Key Findings: Long-Term Functional Superiority
The results of the SECURIS study provide compelling evidence for the benefit of eCAS. At both 90 days and the one-year mark, patients in the eCAS group demonstrated significantly better functional recovery. Specifically, the common odds ratio (cOR) for a one-point improvement on the mRS at one year was 1.47 (95% CI 1.16-1.85, p = 0.001) in favor of stenting.
Enhanced Recanalization Rates
One of the most striking findings was the impact of stenting on technical success. The eCAS group achieved successful recanalization at a rate significantly higher than the non-eCAS group (OR 4.28, 95% CI 2.61-7.0, p < 0.001). This suggests that stabilizing the proximal lesion with a stent not only prevents re-occlusion during the procedure but also provides a more definitive restoration of flow, which is a critical determinant of clinical outcome.
Safety and Hemorrhagic Risk
Crucially, the improved efficacy did not come at the cost of safety. There was no statistically significant difference in the rates of hemorrhagic transformation or symptomatic intracranial hemorrhage between the two groups. Furthermore, mortality rates at 90 days and one year were comparable, alleviating long-standing fears that acute stenting and the required antiplatelet regimens would lead to catastrophic bleeding in the infarct zone.
The Role of Antiplatelet Therapy
The study highlighted the importance of pharmacological management. Within the eCAS cohort, patients who were on dual antiplatelet therapy (DAPT) at 24 hours post-procedure had significantly higher rates of favorable functional outcomes (54.6% vs 22.9%, p < 0.001). This reinforces the concept that the success of eCAS is inextricably linked to appropriate antithrombotic protocols to maintain stent patency while balancing the risk of HT.
Expert Commentary: Interpreting the Data
The SECURIS study provides Class II evidence that supports a more proactive approach to tandem lesions. The finding that eCAS is beneficial even in moderate (50-69%) stenosis is particularly noteworthy, as some practitioners previously reserved stenting only for near-total occlusions. By stabilizing the plaque acutely, clinicians may prevent early recurrent embolization and hemodynamic instability.
However, the study also raised intriguing questions regarding patient selection. Stratified analyses suggested potential differences in treatment effects based on sex and age. While the overall trend favored eCAS, the benefit appeared more pronounced in certain subgroups, suggesting that a personalized approach—considering the patient’s biological age and vascular anatomy—remains essential. The observational nature of the registry, despite the use of IPTW, means that unmeasured confounders could still influence the results, and randomized controlled trials (RCTs) remain the gold standard for definitive confirmation.
Mechanistic Insights: Why Stenting Works
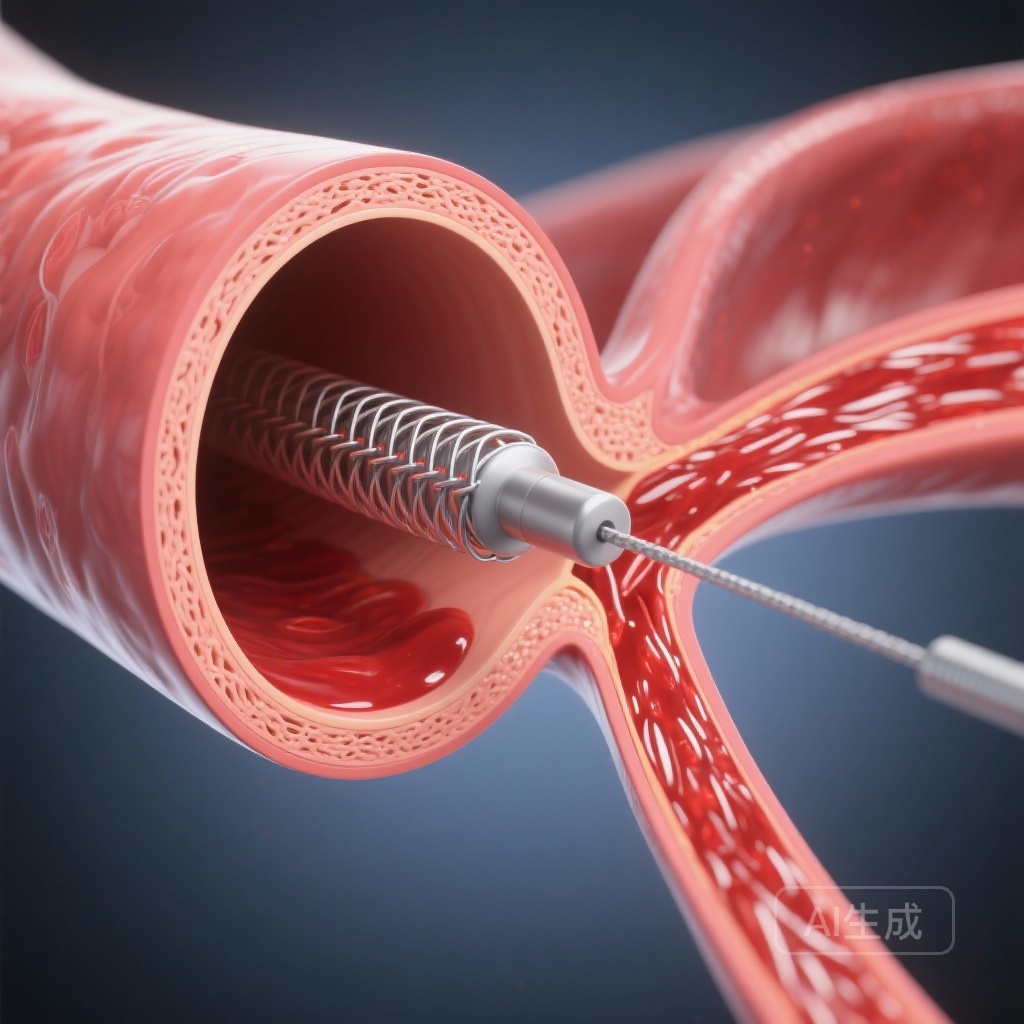
The biological plausibility of eCAS in the acute setting rests on two pillars: flow stabilization and the prevention of re-embolization. Tandem lesions are inherently unstable; a ruptured or severely stenotic carotid plaque serves as a continuous source of emboli. Simple balloon angioplasty without stenting often results in elastic recoil or flow-limiting dissections. By placing a stent, the interventionalist creates a smooth lumen, traps the underlying thrombus or debris against the vessel wall, and ensures consistent cerebral perfusion, which is vital for the survival of the ischemic penumbra.
Conclusion and Clinical Implications
The one-year follow-up results from the SECURIS study mark a significant milestone in our understanding of tandem lesion management. The data suggest that emergent carotid artery stenting is not only safe but provides lasting functional benefits that persist well beyond the acute phase. For clinicians, this study supports the integration of eCAS into the standard endovascular workflow for AIS patients with tandem pathology.
Moving forward, future research should focus on optimizing the timing and dosage of antiplatelet agents in the hyperacute phase and investigating the long-term patency of stents placed under emergency conditions. For now, the SECURIS study offers strong evidence that “fixing the pipe” at the source leads to better lives for stroke survivors.
References
- Ezcurra-Díaz G, Cardona P, et al. Emergent Carotid Artery Stenting in Patients With Acute Ischemic Stroke With Tandem Lesions: One-Year Follow-Up Results From the SECURIS Study. Neurology. 2025 Oct;105(7):e214067.
- Papanagiotou P, White CJ. Endovascular Treatment of Tandem Occlusions in Acute Ischemic Stroke. JACC: Cardiovascular Interventions. 2020;13(15):1745-1747.
- Jovin TG, et al. Endovascular therapy for tandem anterior circulation occlusive disease: pooled analysis from the STRATIS registry. Journal of NeuroInterventional Surgery. 2019;11(12):1187-1191.