Highlighting Superiority of Emergent Carotid Stenting in Tandem Lesions
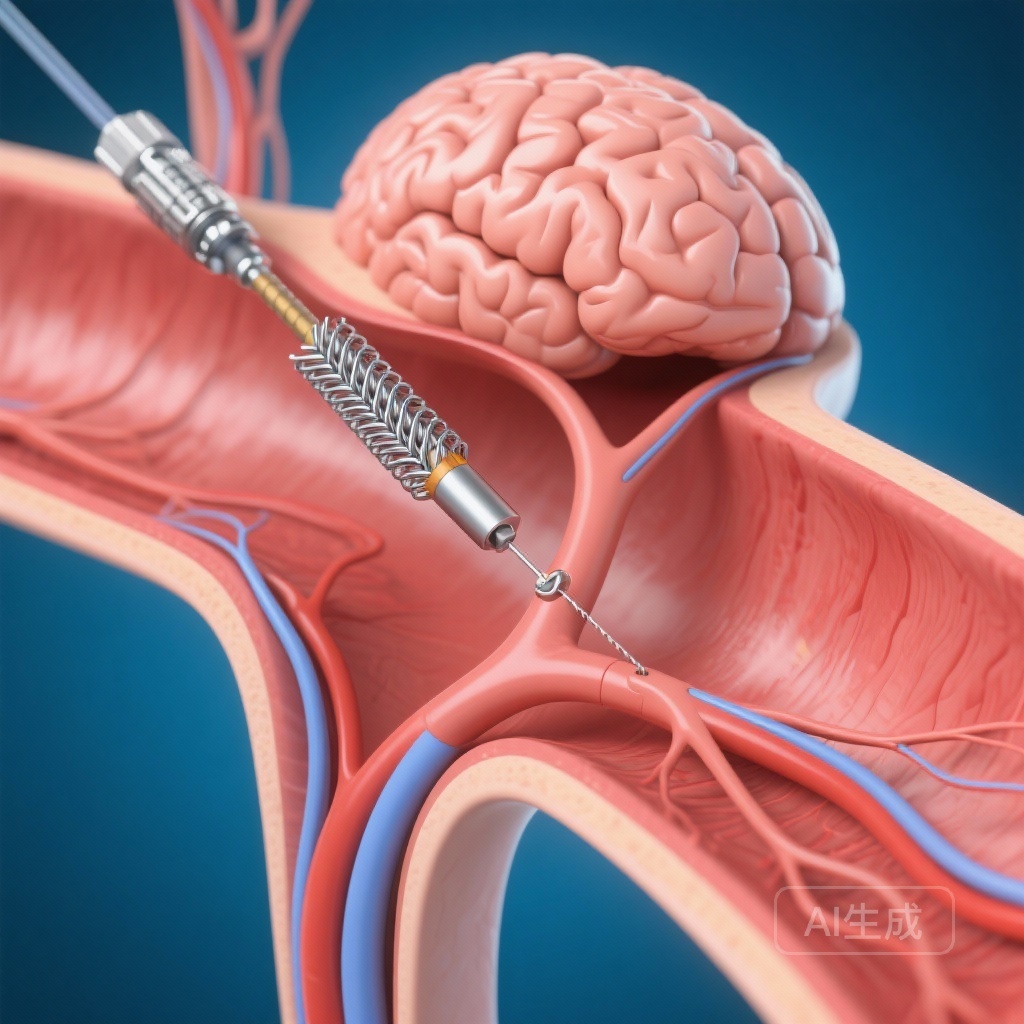
In the evolving landscape of acute ischemic stroke management, tandem lesions—defined as a concomitant high-grade stenosis or occlusion of the extracranial internal carotid artery (ICA) and a downstream intracranial large vessel occlusion (LVO)—represent a significant therapeutic challenge. These lesions occur in approximately 15% to 25% of patients presenting with anterior circulation strokes and are associated with a poorer prognosis compared to isolated intracranial occlusions when treated with thrombolysis alone. While endovascular thrombectomy (EVT) is the established standard of care for LVOs, the optimal management of the proximal carotid lesion during the emergent procedure has remained a subject of intense debate among neuro-interventionalists and stroke neurologists.
The multicenter CERES-TANDEM study, recently published in Neurology, provides critical insights into this clinical dilemma. By analyzing a massive real-world cohort, the study offers robust evidence that emergent carotid stenting (eCAS) during the thrombectomy procedure is associated with significantly better 90-day functional recovery compared to a no-stenting strategy, without a concomitant increase in safety risks. This finding marks a potential shift in the clinical paradigm for treating this complex patient population.
Background: The Clinical Dilemma of Tandem Lesions
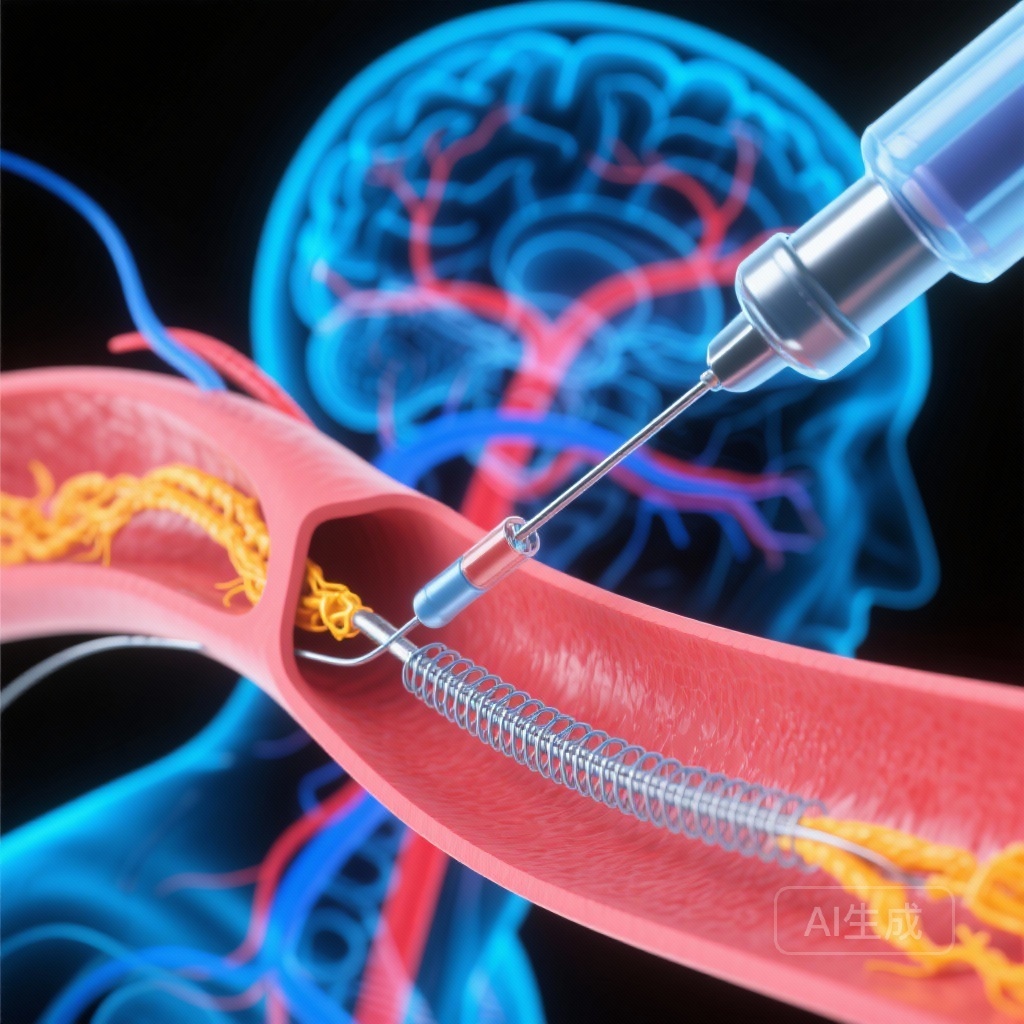
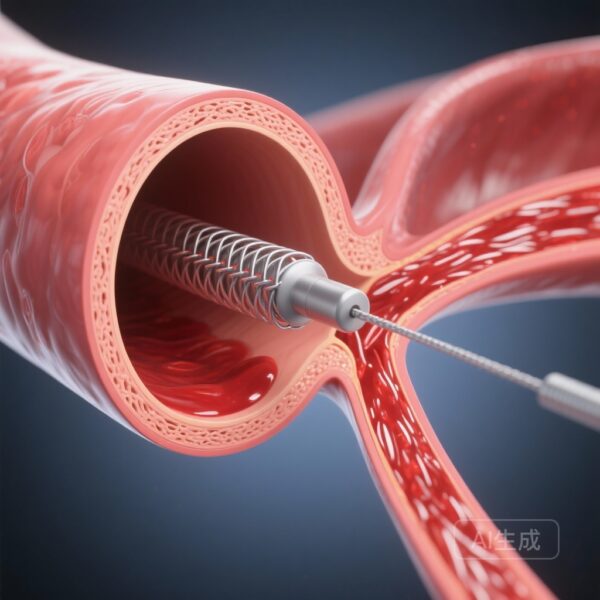
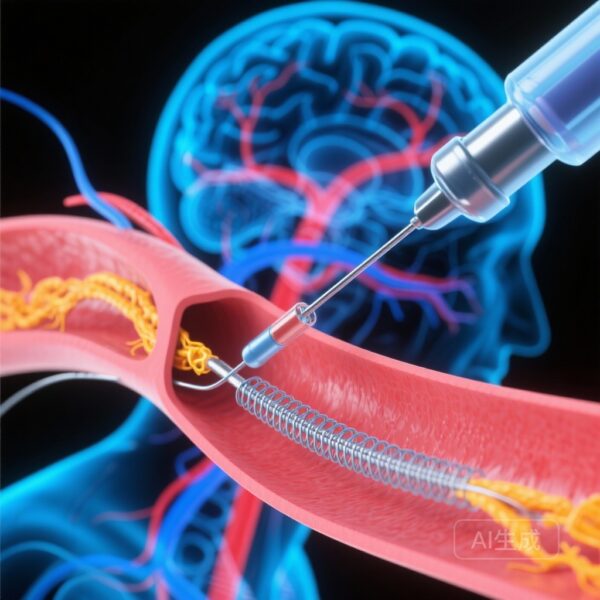
Treatment of tandem lesions requires a dual approach: addressing the distal intracranial occlusion to achieve reperfusion and managing the proximal carotid lesion to ensure sustained blood flow and prevent re-occlusion. Interventionalists typically choose between three strategies for the extracranial lesion: balloon angioplasty alone, emergent carotid stenting (eCAS), or conservative management (treating the intracranial lesion only).
The hesitation surrounding eCAS primarily stems from the necessity of immediate potent antiplatelet therapy to prevent stent thrombosis. In the hyperacute phase of a stroke, where the blood-brain barrier may be compromised and intravenous thrombolysis (IVT) might have been administered, there is a legitimate concern that aggressive antiplatelet use could increase the risk of symptomatic intracranial hemorrhage (sICH). Consequently, many randomized controlled trials (RCTs) of thrombectomy either excluded tandem lesions or were underpowered to provide definitive guidance on the extracranial component. This evidentiary gap led to the initiation of the CERES-TANDEM study.
Study Design and Methodology: The CERES-TANDEM Framework
The CERES-TANDEM study (NCT06965036) was designed as an international multicenter longitudinal retrospective cohort study. It pooled data from 4,053 consecutive adult patients treated across 49 comprehensive stroke centers in Europe, North America, and Singapore between January 2018 and December 2024. This timeframe captures the modern era of thrombectomy devices and techniques.
The study included patients with acute anterior circulation ischemic stroke due to tandem lesions who underwent EVT. Key exclusion criteria were primary hemorrhagic stroke, absence of intracranial occlusion, presentation beyond 24 hours from symptom onset, and pediatric cases. The primary objective was to compare 90-day functional outcomes, measured by the modified Rankin Scale (mRS), between those who received eCAS and those who did not.
To account for the non-randomized nature of the treatment assignment, the researchers employed a sophisticated statistical framework using stabilized inverse probability of treatment weighting (IPTW)-weighted ordinal regression. This method adjusts for baseline imbalances between the treatment groups, mimicking the conditions of a randomized trial. They also analyzed three primary estimands: the mRS shift (Estimand 1), a direct-effect estimand adjusting for successful recanalization and sICH (Estimand 2), and a stratum estimand restricted to ‘never-crossers’ (Estimand 3) to ensure the stability of the findings.
Key Findings: Functional Recovery and Safety
Of the 4,053 patients analyzed, the majority (2,522 patients, or approximately 62%) underwent eCAS, while 1,531 received no stenting. The mean age of the cohort was 70 years, and 65.5% were female. The results of the IPTW analysis were compelling across all primary and secondary endpoints.
Superior Functional Outcomes
The primary analysis revealed that eCAS was associated with a significant improvement in 90-day functional outcomes. The common odds ratio (OR) for a shift toward better mRS scores was 1.31 (95% CI 1.17–1.47; p < 0.001). Furthermore, patients treated with eCAS had higher odds of achieving functional independence, defined as mRS 0–2 (OR 1.30; 95% CI 1.13–1.51; p < 0.001), and excellent recovery, defined as mRS 0–1 (OR 1.27; 95% CI 1.08–1.50; p = 0.005).
Safety and Hemorrhagic Risk
Crucially, the study addressed the primary safety concern: symptomatic intracranial hemorrhage. The incidence of sICH did not show a statistically significant increase in the eCAS group compared to the no-stenting group (OR 1.21; 95% CI 0.93–1.56; p = 0.15). This finding is particularly important as it suggests that the benefits of maintaining carotid patency and preventing re-occlusion outweigh the potential risks associated with the required periprocedural antiplatelet regimens.
Subgroup and Sensitivity Analyses
The benefits of eCAS remained consistent across various clinical scenarios. There was no significant interaction found for factors such as the specific site of intracranial occlusion, the use of intravenous thrombolysis, the sedation technique (general anesthesia vs. conscious sedation), the specific EVT approach (stent retriever vs. aspiration), or the arterial access site (femoral vs. radial). A sensitivity analysis that included successful recanalization (TICI 2b or higher) in the IPTW framework confirmed that eCAS independently contributed to improved outcomes (OR 1.14, p = 0.008).
Expert Commentary: Interpreting Class II Evidence
The CERES-TANDEM study provides Class II evidence, indicating that eCAS is likely beneficial for patients with tandem lesions. From a clinical perspective, these findings suggest that the acute placement of a stent is not merely a technical option but a preferred strategy for maximizing recovery. The higher rate of functional independence in the stenting group may be attributed to improved cerebral hemodynamics and a reduced rate of early recurrent stroke or intracranial re-occlusion.
However, several nuances remain. The study’s retrospective nature, despite the rigorous IPTW adjustment, cannot entirely eliminate the possibility of unmeasured confounding factors, such as the specific choice of antiplatelet agents (e.g., aspirin, clopidogrel, or glycoprotein IIb/IIIa inhibitors) and their timing. Interventionalists often face a ‘balancing act’ between preventing stent thrombosis and avoiding hemorrhagic transformation. Future research should focus on optimizing these pharmacological protocols.
Furthermore, while eCAS showed superiority, the ‘no-stenting’ group in this study was heterogeneous, including patients who may have received angioplasty alone. The distinction between angioplasty and stenting is a critical area for future randomized trials, such as the ongoing EASI (NCT03983447) and TITAN (NCT03978988) trials, which will provide the Class I evidence needed to definitively cement these findings into international guidelines.
Conclusion: Clinical Implications for Stroke Centers
The CERES-TANDEM study represents the largest real-world evaluation of tandem lesion management to date. Its findings strongly support the use of emergent carotid stenting during endovascular thrombectomy for acute anterior circulation ischemic stroke. By demonstrating a significant improvement in 90-day functional outcomes without increasing the risk of symptomatic hemorrhage, the study provides clinicians with the confidence to pursue definitive extracranial intervention during the primary procedure.
For comprehensive stroke centers, these results emphasize the importance of having standardized protocols for tandem lesion management, including the availability of carotid stents and established antiplatelet strategies. While we await the results of dedicated randomized controlled trials, the CERES-TANDEM data suggests that for most patients with tandem lesions, ‘fixing the pipe’ at the source is a vital component of successful neurovascular rescue.
Funding and Clinical Trials
The CERES-TANDEM study is registered at clinicaltrials.gov under the identifier NCT06965036. No specific external funding was reported for the retrospective data collection across the 49 participating centers, reflecting a collaborative international effort to improve stroke care standards.
References
1. Romoli M, Molina CA, Zapata-Arriaza E, et al. Emergent Carotid Stenting for Acute Anterior Circulation Ischemic Stroke With Tandem Lesions: The Multicenter CERES-TANDEM Study. Neurology. 2026;106(2):e214528. doi:10.1212/WNL.0000000000214528.
2. Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387(10029):1723-1731.
3. Papanagiotou P, White AJ. Treatment of Tandem Occlusions: A Review of Current Management. Frontiers in Neurology. 2020;11:568.