Introduction: The Hidden Neurovascular Risks of Hypertensive Pregnancy
Hypertensive disorders of pregnancy (HDP), including preeclampsia and gestational hypertension, are increasingly recognized not merely as transient obstetric complications but as early markers of lifelong cardiovascular and cerebrovascular disease. Research has consistently shown that women with a history of HDP face a significantly higher risk of stroke, cognitive decline, and dementia later in life. Imaging studies have previously identified structural brain changes, such as reduced volumes of gray and white matter and an increased burden of white matter hyperintensities, in women years after a hypertensive pregnancy. However, until recently, it remained unclear whether these structural changes are irreversible or if early intervention during the critical postpartum period could mitigate damage and promote neurovascular recovery.
Highlighting the POP-HT Trial
1. Intensive postpartum blood pressure (BP) management using telemonitoring and physician-guided titration led to significantly larger total white matter volumes compared to usual care at nine months post-delivery.
2. Women in the usual care group who experienced preeclampsia showed significantly smaller subcortical volumes (putamen, accumbens, and pallidum) compared to those with gestational hypertension; notably, this difference was absent in the intervention group.
3. The findings suggest that the first months post-partum represent a ‘golden window’ for neuroprotective strategies through optimized hemodynamic control.
The POP-HT Imaging Substudy: Design and Methodology
The Physician Optimized Postpartum blood pressure self-management trial (POP-HT) was a prospective, open-label, randomized clinical trial conducted at a single tertiary center in the United Kingdom. The primary aim of the parent trial was to investigate whether a telemonitored self-management intervention could lower blood pressure in the postpartum period. This specific substudy focused on secondary imaging outcomes to determine if such BP optimization influenced brain structure.
Participant Characteristics
Participants were recruited if they were older than 18 years and had been diagnosed with preeclampsia or gestational hypertension requiring antihypertensive medication at the time of hospital discharge. A total of 252 participants were eligible, and 220 were randomized. For the imaging substudy, T1-weighted magnetic resonance imaging (MRI) data were available for 157 participants at approximately nine months postpartum.
The Intervention
The intervention group received a telemonitored self-management program. This included a home BP monitor and a dedicated app that allowed participants to upload readings. Research physicians reviewed these data and guided the titration of antihypertensive medications to achieve target BP levels. In contrast, the usual care group followed standard postnatal protocols, which typically involve BP checks by community midwives or general practitioners with less frequent medication adjustments.
Imaging Analysis
Brain volumes, including total gray matter, white matter, cerebrospinal fluid, and specific subcortical structures (such as the hippocampus, putamen, and thalamus), were measured using automated segmentation. All analyses were adjusted for total intracranial volume to ensure that differences in head size did not confound the results.
Key Findings: Structural Preservation Through BP Control
The results of the POP-HT substudy provide compelling evidence that early intervention alters the structural trajectory of the brain following a hypertensive pregnancy.
White Matter Volume Preservation
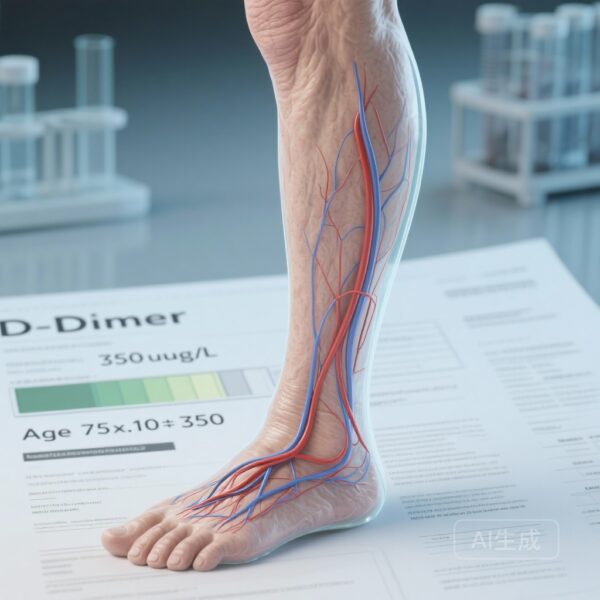
The most significant finding was that the intervention group (n = 81) exhibited larger total white matter volumes compared to the usual care group (n = 71). The adjusted mean difference was 11.50 cm3 (95% CI, 2.04 to 20.96; P = .02). White matter is crucial for the connectivity of the brain, and its preservation is strongly linked to maintaining cognitive processing speed and preventing future vascular dementia.
Protection Against Subcortical Atrophy
The study also highlighted a specific vulnerability in women who experienced preeclampsia. In the usual care group, those with preeclampsia had significantly smaller volumes in key subcortical regions compared to those with gestational hypertension:
– Putamen: Adjusted mean difference, -0.83 cm3 (P < .001)
– Accumbens: Adjusted mean difference, -0.15 cm3 (P = .003)
– Pallidum: Adjusted mean difference, -0.13 cm3 (P = .04)
Crucially, these volume deficits were not observed in the intervention group. This suggests that the intensive BP management intervention effectively 'leveled the playing field,' protecting the brains of women with preeclampsia from the structural loss typically associated with the condition.
Expert Commentary: Mechanistic Insights and Clinical Significance
The physiological mechanisms underlying these findings are likely multifactorial. Hypertensive pregnancy is associated with endothelial dysfunction, systemic inflammation, and blood-brain barrier (BBB) disruption. The sudden hemodynamic shifts during and after delivery can exacerbate these issues, leading to cerebral edema or small vessel injury. By optimizing BP early in the postpartum period, clinicians may be reducing the ‘hemodynamic stress’ on the cerebral vasculature, allowing the BBB to repair and preventing the downstream loss of neural tissue.
Limitations and Considerations
While these results are promising, certain limitations must be acknowledged. This was a single-center study, and the participant population may not represent all demographic groups. Furthermore, while brain volume is a well-validated surrogate marker for brain health and cognitive reserve, long-term follow-up is required to confirm whether these structural differences translate into a reduced incidence of clinical stroke or dementia in the decades to follow.
Conclusion: A New Standard for Postpartum Care?
The POP-HT imaging substudy shifts the narrative of postpartum care from simple safety monitoring to proactive long-term health optimization. It demonstrates that the neurological consequences of hypertensive pregnancy are not entirely fixed at the time of delivery. Instead, the postpartum period offers a therapeutic opportunity to intervene and potentially alter a woman’s neurovascular aging trajectory.
For clinicians, these findings underscore the importance of rigorous BP management in the weeks and months following a hypertensive pregnancy. Moving toward telemonitored, physician-guided titration models could provide a scalable and effective method to protect both the cardiovascular and neurological health of this high-risk population.
Funding and Trial Registration
This study was funded by various grants and supported by the NIHR Oxford Biomedical Research Centre. The trial is registered at ClinicalTrials.gov (Identifier: NCT04273854).
References
Lapidaire W, Kitt J, Krasner S, et al. Brain Volumes After Hypertensive Pregnancy and Postpartum Blood Pressure Management: A POP-HT Randomized Clinical Trial Imaging Substudy. JAMA Neurol. 2026 Jan 5. doi:10.1001/jamaneurol.2025.5145. PMID: 41490362.