Highlight
Strong Association Between OSA and PD
In a longitudinal study involving over 11 million veterans, patients diagnosed with obstructive sleep apnea (OSA) exhibited a significantly higher risk of developing incident Parkinson disease (PD) compared to those without the sleep disorder.
Neuroprotective Potential of Early CPAP
Continuous positive airway pressure (CPAP) therapy, when initiated early in the course of OSA, was associated with a marked reduction in the cumulative incidence of PD, suggesting a window of opportunity for clinical intervention.
Sex-Specific Risk Magnitudes
While OSA increased PD risk across the cohort, the magnitude of this association was notably greater in female veterans, highlighting the need for sex-sensitive screening and treatment protocols.
Introduction: The Intersection of Sleep and Neurodegeneration
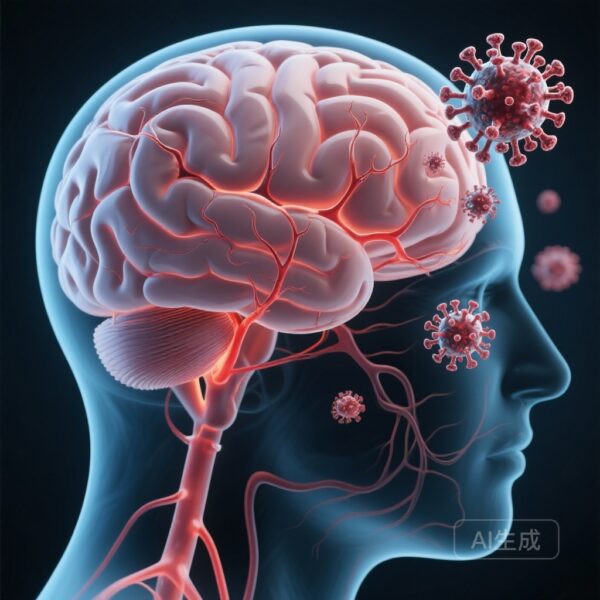
Obstructive sleep apnea (OSA) is increasingly recognized not merely as a respiratory condition, but as a systemic disorder with profound implications for brain health. Characterized by repetitive episodes of upper airway collapse during sleep, OSA leads to intermittent hypoxia, sleep fragmentation, and intrathoracic pressure fluctuations. While its links to cardiovascular disease and metabolic syndrome are well-established, its role in neurodegenerative processes—specifically Parkinson disease (PD)—has remained a subject of intense debate and conflicting data.
Parkinson disease is the second most common neurodegenerative disorder worldwide, characterized by the progressive loss of dopaminergic neurons in the substantia nigra. Growing evidence suggests that sleep disturbances are not just comorbid symptoms of PD but may actually precede motor symptoms by years, potentially serving as a prodromal driver. A new study published in JAMA Neurology by Neilson et al. provides the most robust evidence to date regarding the temporal relationship between OSA and PD and, crucially, the impact of treatment on this trajectory.
Study Design: A Massive EHR-Based Veteran Cohort
To address the limitations of prior, smaller studies, researchers conducted a retrospective cohort study using electronic health records (EHR) from the United States Veterans Affairs (VA) health system. The study period spanned over two decades, from January 1, 1999, to December 30, 2022.
Population and Methodology
After screening over 13.7 million veterans, the final analysis included 11,310,411 individuals. The mean age was 60.5 years, with a follow-up average of nearly five years. The researchers excluded any patients who already had a PD diagnosis at the time of OSA exposure to ensure a clear temporal sequence. OSA was identified through administrative ICD codes, while CPAP usage data was meticulously extracted from semistructured medical interview fields within the EHR.
Statistical Rigor
One of the strengths of this study was its approach to confounding. The primary outcome—cumulative incidence of PD—was calculated while adjusting for the competing risk of death. The models balanced for age, race, sex, and smoking status, and were further adjusted for body mass index (BMI), vascular comorbidities (such as hypertension and diabetes), psychiatric conditions, and relevant medications that might influence neurological outcomes.
Key Findings: Quantifying the OSA-PD Link
Among the 1.55 million veterans diagnosed with OSA, the data revealed a clear and statistically significant increase in the risk of incident Parkinson disease.
Incidence Rates
Veterans with OSA demonstrated an additional 1.61 cases of PD per 1000 people (95% CI, 1.13-2.09) at six years post-diagnosis compared to those without OSA. This finding suggests that OSA is an independent risk factor for PD, even after accounting for the various comorbidities that often cluster with sleep-disordered breathing.
Sex-Based Disparities
An intriguing finding of the study was the sex-specific difference in risk. Although the majority of the veteran cohort was male, the relative increase in PD risk associated with OSA was significantly higher in female veterans. This observation aligns with a growing body of literature suggesting that women may be more susceptible to the neurological consequences of sleep fragmentation or that the pathophysiological manifestation of OSA in women carries different risks for neurodegeneration.
The Protective Role of Early CPAP Therapy
Perhaps the most clinically actionable finding of the Neilson et al. study is the impact of CPAP therapy. CPAP is the gold standard for treating OSA, providing a pneumatic splint to the airway to prevent collapse.
The researchers found that when CPAP was initiated early in the disease course, the cumulative incidence of PD was significantly reduced. This suggests that the pathological mechanisms triggered by OSA—such as oxidative stress, neuroinflammation, and impaired waste clearance—may be reversible or at least mitigatable if the respiratory disturbance is corrected promptly. The reduction in case numbers among the CPAP-treated group highlights a potential paradigm shift: treating OSA may not just improve quality of life and cardiovascular health, but may also serve as a neuroprotective strategy.
Expert Commentary: Biological Plausibility and Mechanistic Insights
Why would a respiratory condition like OSA lead to Parkinson disease? Several biological mechanisms have been proposed to explain this link.
The Glymphatic System and Protein Clearance
During deep sleep, the brain’s glymphatic system—a macroscopic waste clearance pathway—is most active, flushing out metabolic byproducts like alpha-synuclein. OSA severely disrupts sleep architecture, particularly slow-wave sleep. It is hypothesized that the sleep fragmentation seen in OSA impairs this clearance mechanism, allowing for the accumulation of toxic protein aggregates that are the hallmark of PD.
Intermittent Hypoxia and Oxidative Stress
Repetitive oxygen desaturation followed by reoxygenation (intermittent hypoxia) is a potent trigger for oxidative stress. The dopaminergic neurons in the substantia nigra are known to be particularly vulnerable to oxidative damage due to their high metabolic demand and unique physiological structure. The chronic inflammatory state induced by OSA may accelerate the degeneration of these sensitive neurons.
Blood-Brain Barrier Integrity
Chronic sleep apnea has been shown to compromise the integrity of the blood-brain barrier (BBB). A leaky BBB can allow peripheral inflammatory cytokines and toxins to enter the central nervous system, further fueling neuroinflammatory processes that contribute to dopaminergic cell death.
Study Limitations and Considerations
While the study’s scale is unprecedented, certain limitations must be acknowledged. As an EHR-based retrospective study, it relies on the accuracy of administrative coding. Furthermore, CPAP adherence is notoriously difficult to track accurately outside of controlled settings; the study relied on medical interview data, which may be subject to recall bias. Additionally, the veteran population, while diverse, is predominantly male and may have higher rates of other risk factors, such as traumatic brain injury or toxic exposures, which could interact with OSA in complex ways.
Conclusion: A New Frontier in Preventive Neurology
The study by Neilson and colleagues represents a significant step forward in our understanding of the relationship between sleep and neurodegeneration. By demonstrating that OSA is a modifiable risk factor for Parkinson disease, the research provides a clear mandate for clinicians.
For primary care physicians and sleep specialists, the findings underscore the importance of early screening and aggressive management of OSA. For neurologists, it suggests that assessing sleep quality and respiratory health should be a standard component of the neurological exam, particularly in patients showing early signs of PD or those with a high risk profile. Effective protocols for ensuring long-term CPAP adherence may eventually be viewed as a cornerstone of brain health maintenance in the aging population.
References
1. Neilson LE, Montaño I, May JL, et al. Obstructive Sleep Apnea, Positive Airway Pressure, and Implications of Early Treatment in Parkinson Disease. JAMA Neurol. 2025 Nov 24:e254691.
2. Bohnen NI, Hu MT. Sleep Disturbance as Potential Main Driver of PD Pathogenesis. Mov Disord. 2019;34(11):1600-1608.
3. Shpirer I, et al. Sleep apnea and Parkinson’s disease. Sleep Med. 2012;13(7):893-897.
4. Postuma RB, et al. Risk and predictors of Parkinson’s disease in patients with REM sleep behavior disorder. Lancet Neurol. 2015;14(3):310-321.