Highlight
The SKYSCRAPER-08 trial represents a significant milestone in the treatment of esophageal squamous cell carcinoma (ESCC). Key highlights include:
- Significant improvement in median overall survival (OS): 15.7 months with the dual-checkpoint combination versus 11.1 months with chemotherapy alone (HR 0.70).
- Substantial reduction in the risk of disease progression or death: Progression-free survival (PFS) hazard ratio of 0.56, indicating a 44% improvement.
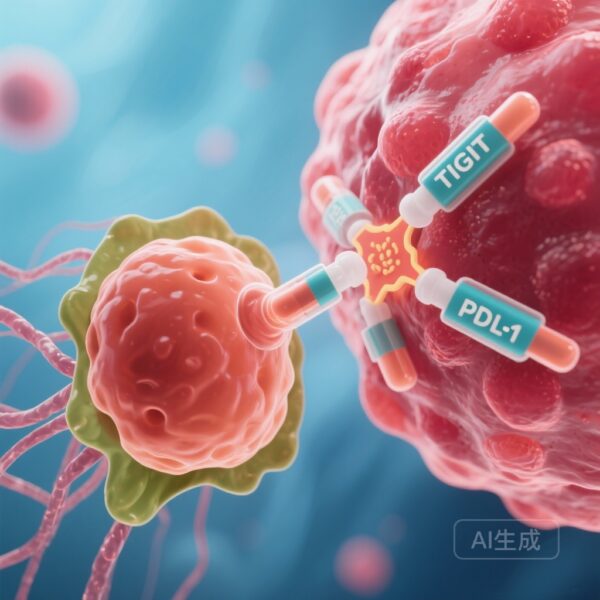
- The first Phase 3 trial to validate the efficacy of combining an anti-TIGIT agent (tiragolumab) with an anti-PD-L1 agent (atezolizumab) and chemotherapy in a first-line ESCC setting.
- Manageable safety profile with no new safety signals, despite a slight increase in immune-mediated adverse events.
Background and Disease Burden
Esophageal cancer remains one of the most challenging malignancies to treat globally, with esophageal squamous cell carcinoma (ESCC) being the predominant histological subtype, particularly in Asian populations. For patients presenting with unresectable locally advanced or metastatic disease, the prognosis has historically been poor, with five-year survival rates often falling below 5%. While the introduction of PD-1 inhibitors in combination with chemotherapy has improved outcomes and become a standard of care, many patients still experience disease progression, underscoring an urgent unmet need for more potent therapeutic strategies.
The TIGIT (T-cell immunoreceptor with Ig and ITIM domains) pathway has emerged as a promising target for cancer immunotherapy. TIGIT is an inhibitory receptor expressed on T cells and natural killer (NK) cells that contributes to immune evasion by tumors. By blocking both the TIGIT and PD-L1 pathways, researchers hypothesized a synergistic effect that could reinvigorate the anti-tumor immune response more effectively than single-pathway inhibition. The SKYSCRAPER-08 trial was designed to test this hypothesis in a first-line setting for ESCC.
Study Design: The SKYSCRAPER-08 Framework
SKYSCRAPER-08 was a randomized, double-blind, placebo-controlled, Phase 3 trial conducted across 67 specialized centers in mainland China, South Korea, Thailand, Taiwan, and Hong Kong. The trial enrolled 461 treatment-naive adult patients with unresectable locally advanced, recurrent, or metastatic ESCC and an ECOG performance status of 0-1.
Participants were randomly assigned in a 1:1 ratio to receive either:
- The Investigational Arm: Tiragolumab (600 mg) plus atezolizumab (1200 mg) combined with chemotherapy (paclitaxel 175 mg/m2 and cisplatin 60-80 mg/m2).
- The Control Arm: Placebo plus the same chemotherapy regimen.
Treatment was administered via intravenous infusion in 21-day cycles for up to six cycles of chemotherapy, followed by maintenance with the assigned immunotherapy or placebo. The co-primary endpoints were progression-free survival (PFS) as assessed by an independent review facility (IRF) and overall survival (OS) in the intention-to-treat (ITT) population.
Key Findings: Efficacy and Survival Data
The results of SKYSCRAPER-08 demonstrated a statistically significant and clinically meaningful improvement across both primary endpoints. At the time of the primary PFS analysis (cutoff June 15, 2022), the median PFS in the tiragolumab-atezolizumab-chemotherapy group was 6.2 months (95% CI 5.7–7.2) compared to 5.4 months (95% CI 4.4–5.5) in the placebo-chemotherapy group. This translated to a hazard ratio (HR) of 0.56 (95% CI 0.45–0.70; p < 0.0001), representing a robust delay in disease progression.
The OS data (cutoff Feb 13, 2023) were equally compelling. The median OS was 15.7 months (95% CI 13.3–20.4) for the dual-checkpoint arm versus 11.1 months (95% CI 9.6–13.6) for the control arm. The HR for death was 0.70 (95% CI 0.55–0.88; p=0.0024). These results suggest that the addition of tiragolumab and atezolizumab provides a durable survival benefit that exceeds the current benchmarks for chemotherapy-only regimens.
Safety and Tolerability Profile
The safety profile of the triplet combination was generally consistent with the known effects of the individual agents. Grade 3–4 adverse events occurred at similar rates in both groups: 98% in the investigational group and 96% in the control group. The most frequent high-grade toxicities were hematological, including decreased white blood cell counts and decreased neutrophil counts, which are primarily attributed to the chemotherapy backbone.
Serious adverse events (SAEs) occurred in 41% of patients receiving tiragolumab and atezolizumab compared to 39% in the placebo group. Pneumonia was the most common SAE in both arms. Notably, there were six treatment-related deaths in the investigational arm (3%), including cases of immune-mediated lung disease and pneumonitis, compared to two deaths (1%) in the control arm. While the incidence of immune-related adverse events was higher in the tiragolumab group, they were mostly manageable with standard protocols, and no new safety signals were identified.
Expert Commentary and Clinical Implications
The success of SKYSCRAPER-08 provides the first definitive Phase 3 evidence that TIGIT inhibition, when combined with PD-L1 blockade and chemotherapy, can enhance clinical outcomes in ESCC. Mechanistically, this supports the theory that dual blockade can overcome compensatory immune resistance mechanisms that often limit the efficacy of single-agent checkpoint inhibitors.
Clinicians should note that the trial population was entirely Asian. While ESCC is highly prevalent in Asia, further data may be needed to confirm these findings in Western populations where the etiology and patient demographics might differ. However, given the biological similarities of ESCC across regions, these results are widely considered a major step forward. The trial also highlights the importance of patient selection and monitoring for immune-related toxicities, particularly pneumonitis, when employing multi-agent immunotherapy regimens.
Compared to existing standards like KEYNOTE-590 (pembrolizumab + chemo) and CheckMate 648 (nivolumab + chemo or nivolumab + ipilimumab), SKYSCRAPER-08 offers a competitive survival benefit. The 15.7-month median OS is among the highest reported in a Phase 3 trial for this patient population, positioning the tiragolumab-atezolizumab-chemotherapy combination as a potential new first-line standard of care.
Conclusion
The SKYSCRAPER-08 trial successfully met its primary endpoints, demonstrating that the addition of tiragolumab and atezolizumab to chemotherapy significantly improves PFS and OS in patients with advanced esophageal squamous cell carcinoma. These findings validate the clinical utility of targeting the TIGIT pathway and offer a new therapeutic horizon for a disease with a historically dismal outlook. As the oncology community moves toward more personalized and multi-targeted approaches, SKYSCRAPER-08 serves as a robust foundation for future explorations of dual checkpoint inhibition.
Funding and ClinicalTrials.gov
This study was funded by F. Hoffmann-La Roche-Genentech. The trial is registered with ClinicalTrials.gov, number NCT04540211.
References
- Hsu CH, Lu Z, Gao S, et al. Tiragolumab plus atezolizumab and chemotherapy as first-line treatment for patients with unresectable oesophageal squamous cell carcinoma (SKYSCRAPER-08): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2026 Jan;27(1):103-115.
- Sun JM, Shen L, Shah MA, et al. Pembrolizumab plus chemotherapy versus chemotherapy alone for first-line treatment of advanced oesophageal cancer (KEYNOTE-590): a randomised, placebo-controlled, phase 3 study. Lancet. 2021;398(10302):759-771.
- Doki Y, Ajani JA, Kato K, et al. Nivolumab combinations in advanced esophageal squamous-cell carcinoma. N Engl J Med. 2022;386(5):449-462.