Highlights
The Diabetes Endothelial Keratoplasty Study (DEKS), a large-scale randomized clinical trial, has provided definitive evidence regarding the use of corneal tissue from donors with diabetes. The key highlights include:
- 1-year graft success rates were nearly identical between recipients of tissue from donors with diabetes (97.1%) and those without (96.3%).
- Endothelial cell loss (ECL) at one year post-surgery showed no significant difference, with both groups averaging approximately 28% loss.
- The severity of the donor’s diabetes did not correlate with poorer clinical outcomes, primary graft failure, or altered cell morphometry.
- These findings provide strong clinical support for expanding the corneal donor pool by removing restrictions on tissue from donors with diabetes for DMEK procedures.
Background: Addressing the Donor Shortage in the Era of DMEK
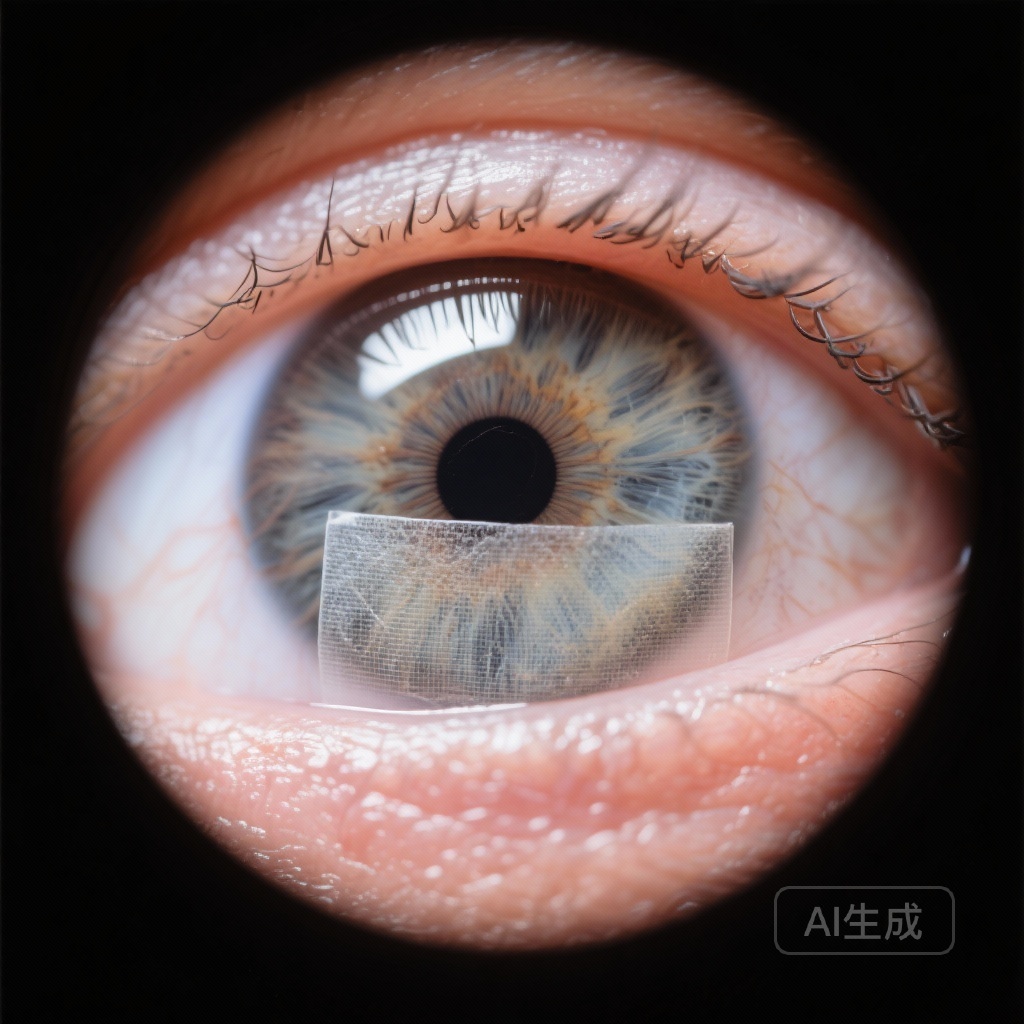
Descemet membrane endothelial keratoplasty (DMEK) has emerged as the gold standard for treating corneal endothelial diseases, such as Fuchs endothelial corneal dystrophy (FECD) and pseudophakic bullous keratopathy. Compared to its predecessor, Descemet stripping automated endothelial keratoplasty (DSAEK), DMEK offers superior visual acuity recovery and lower rejection rates. However, DMEK is technically more demanding, particularly during the preparation of the donor tissue, where the thin Descemet membrane and endothelium must be stripped from the stroma.
Historically, there has been significant hesitation among surgeons and eye banks regarding the use of tissue from donors with diabetes mellitus. This hesitation stems from concerns that diabetic tissue may be more fragile during preparation or that the underlying diabetic state could compromise endothelial cell survival and function post-transplantation. Given the rising global prevalence of diabetes, these restrictions significantly limit the available donor pool. The Diabetes Endothelial Keratoplasty Study (DEKS) was designed to rigorously evaluate whether these concerns are clinically justified.
Study Design and Methodology
The DEKS was a multicenter, double-masked, randomized clinical trial conducted across 28 clinical sites in the United States, involving 46 surgeons and 13 eye banks. The trial aimed to evaluate two primary dimensions of DMEK outcomes: the overall graft success rate and the physiological health of the transplanted endothelium (cell loss and morphometry).
Participants were individuals undergoing low to moderate risk DMEK, with the vast majority (95%) being treated for Fuchs endothelial corneal dystrophy. The study employed a minimization procedure to assign donor tissue, achieving approximately a 2:1 ratio of donors without diabetes to donors with diabetes. The trial was registered under ClinicalTrials.gov (NCT05134480) and followed participants for one year post-operatively.
The study was split into two primary reports. The first focused on the 1-year cumulative probability of graft success, while the second focused on endothelial cell density (ECD), endothelial cell loss (ECL), and morphometric changes (coefficient of variation and hexagonality).
Clinical Outcomes: Graft Success and Failure Rates
In the analysis of 1,421 study eyes from 1,097 individuals, the researchers found that donor diabetes status had no significant impact on the probability of graft success. At the one-year mark, the cumulative probability of graft success was 96.3% for tissue from donors without diabetes and 97.1% for tissue from donors with diabetes. The difference of 0.7 percentage points was statistically insignificant (P = .63).
Furthermore, the study investigated whether the severity of the donor’s diabetes played a role. Using a severity rating scale based on medical history, success rates remained high across all subgroups: 96.5% for mild diabetes and 97.3% for moderate to severe diabetes. Failure rates were also comparable between the two groups. Primary donor failure occurred in 2.5% of the non-diabetic donor group versus 2.6% in the diabetic donor group. Early failures related to surgical complications and subsequent failures were similarly low in both cohorts, and notably, there were no failures attributed to graft rejection during the first year.
Physiological Metrics: Endothelial Cell Density and Morphometry
A secondary but critical concern was whether diabetic tissue would experience accelerated endothelial cell loss (ECL) over time. The analysis of 1,274 eyes with analyzable postoperative images revealed that preoperative endothelial cell densities (ECD) were nearly identical between the two groups (~2,670 cells/mm2). At one year, the mean ECL was 28.3% for the non-diabetic group and 28.0% for the diabetic group.
The resulting 1-year ECD was 1,927 cells/mm2 in the non-diabetic group and 1,920 cells/mm2 in the diabetic group, with an adjusted mean difference of only 10 cells/mm2 (P = .95). Beyond cell density, the study also measured cell morphometry, which serves as an indicator of endothelial health and stability. The coefficient of variation in cell area (CV) and the percentage of hexagonal cells (HEX) showed no significant differences between the groups, regardless of donor diabetes status or severity.
Expert Commentary and Clinical Implications
The results of the DEKS trial provide a robust evidence base for changing clinical practice and eye bank protocols. For years, the ophthalmology community has debated the suitability of diabetic donor tissue for DMEK. While some previous studies suggested that diabetic tissue might be more prone to tearing during preparation or have reduced cell viability, the large-scale, randomized nature of DEKS provides a more definitive answer.
The findings suggest that once a donor cornea is successfully prepared for DMEK—meaning the membrane is intact and the tissue is transplantable—the clinical performance of that tissue is indistinguishable from non-diabetic tissue. While the study did not focus on the “rate of successful preparation” (i.e., how many diabetic tissues are discarded due to preparation tears), it clearly demonstrates that once transplanted, the diabetic graft is equally successful.
This has profound implications for the global supply of transplantable corneas. As the aging population increases the demand for endothelial keratoplasty, and the prevalence of diabetes continues to rise, being able to confidently use diabetic donor tissue will prevent unnecessary tissue wastage and reduce waiting times for patients.
Conclusion
In conclusion, the Diabetes Endothelial Keratoplasty Study demonstrates that donor diabetes status does not negatively affect the 1-year success rate, endothelial cell density, or cell morphometry following DMEK. Whether the donor had mild or severe diabetes, the outcomes for recipients remained excellent and comparable to those receiving non-diabetic tissue. These findings support a paradigm shift toward more inclusive donor selection criteria, ensuring that more patients can benefit from the visual recovery offered by DMEK.
Funding and ClinicalTrials.gov
The study was supported by grants from the National Eye Institute of the National Institutes of Health. ClinicalTrials.gov Identifier: NCT05134480.
References
1. Lass JH, Benetz BA, Verdier DD, et al. Endothelial Cell Loss 1 Year After Successful DMEK in the Diabetes Endothelial Keratoplasty Study: A Randomized Clinical Trial. JAMA Ophthalmol. 2025;143(12):1053-1060. doi:10.1001/jamaophthalmol.2025.4261.
2. Price FW Jr, Szczotka-Flynn LB, Price MO, et al. Donor Diabetes and 1-Year Descemet Membrane Endothelial Keratoplasty Success Rate: A Randomized Clinical Trial. JAMA Ophthalmol. 2025;143(12):1043-1051. doi:10.1001/jamaophthalmol.2025.4253.