Highlights
- Disitamab Vedotin (DV), a HER2-targeted antibody-drug conjugate, in combination with gemcitabine, achieves a 50% overall pathological complete response (pCR) rate in HER2-positive muscle-invasive bladder cancer (MIBC).
- Four treatment cycles result in higher pCR rates compared to three cycles (69% vs. 31%).
- Toxicity profile is manageable, with most adverse events being mild to moderate and reversible.
- Findings address an urgent need for cisplatin-free neoadjuvant options in patients with comorbidities or renal impairment.
Background
Muscle-invasive bladder cancer (MIBC) represents a significant therapeutic challenge due to its aggressive nature and high risk of recurrence. The current standard of care for eligible patients includes cisplatin-based neoadjuvant chemotherapy followed by radical cystectomy (RC). However, cisplatin is contraindicated in a substantial proportion of patients, particularly those with renal dysfunction, ototoxicity, cardiac comorbidities, or other severe health conditions. The identification of alternative effective regimens is a pressing need.
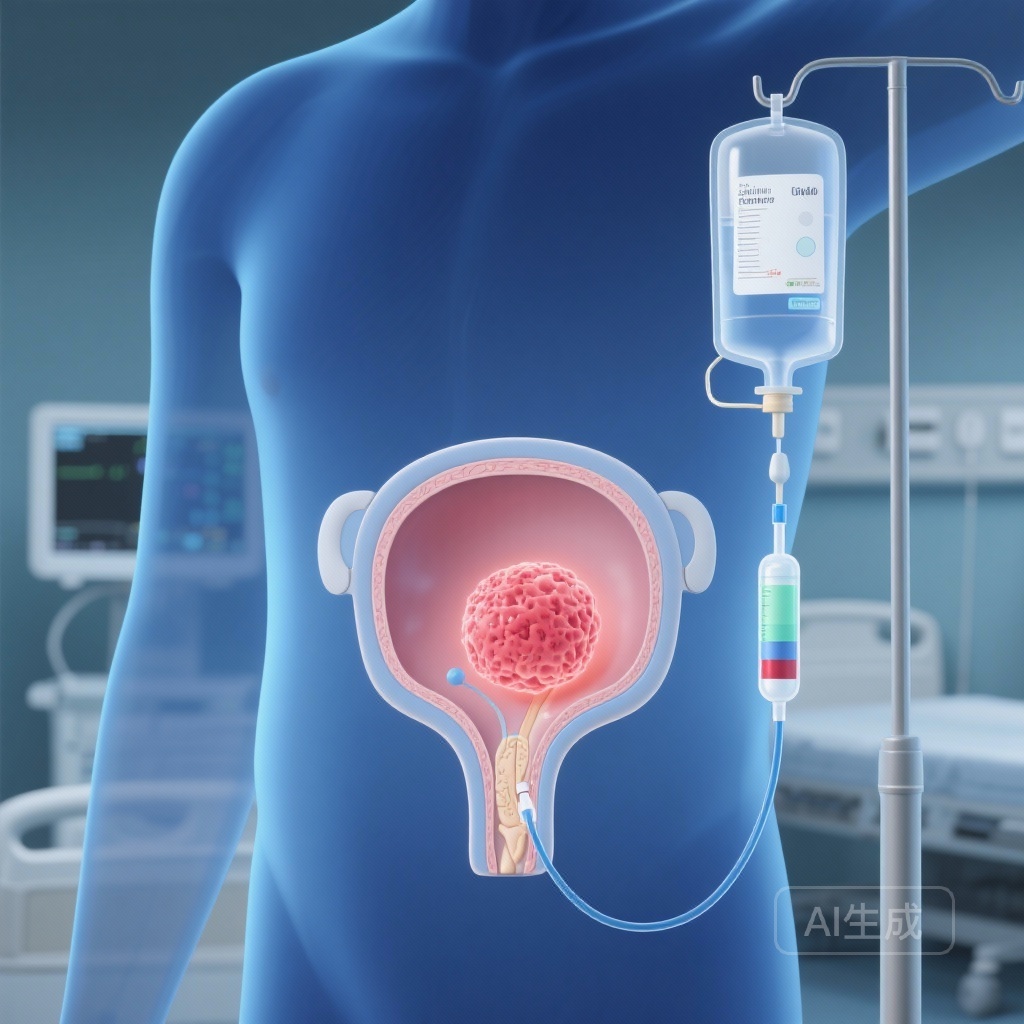
HER2 overexpression in urothelial carcinoma has emerged as a potential therapeutic target. Disitamab Vedotin (DV, also known as RC48) is an antibody-drug conjugate that delivers a cytotoxic payload specifically to HER2-expressing cells. Preclinical and early-phase clinical data have demonstrated promising efficacy in HER2-positive urothelial cancer, prompting exploration of DV in earlier disease settings.
Study Design
This open-label, multicenter, single-arm phase 2 trial enrolled 26 patients with clinical stage T2–T4a Nx M0 MIBC and confirmed HER2 immunohistochemistry scores of 2+ or 3+. The neoadjuvant regimen comprised DV at 2 mg/kg intravenously on day 1, followed by gemcitabine at 1000 mg/m² intravenously on day 2, in a 14-day cycle. Thirteen patients received three cycles, and 13 patients received four cycles, based on clinical discretion and patient tolerance. The primary endpoint was pathological complete response (pCR) rate. Secondary endpoints included safety profile, surgical feasibility, and event-free survival.
Key Findings
Efficacy
Among the 22 patients who underwent RC, the postoperative pathology revealed a pCR rate of 59% (13/22). In cycle stratification, the pCR rate was 40% (4/10) for those who received three cycles and 75% (9/12) for those who completed four cycles. When analyzed by intention-to-treat including all enrolled patients, the overall pCR rate was 50% (13/26), with 31% (4/13) in the three-cycle group and 69% (9/13) in the four-cycle group. Notably, the higher pCR rate with four cycles suggests a dose-intensity relationship and potential cumulative benefit.
At a median follow-up of 16.9 months, 25 out of 26 patients remained event-free, indicating potential durability of the neoadjuvant effect.
Safety
Adverse events were predominantly mild-to-moderate and did not require discontinuation in most cases. The most common treatment-related toxicities included elevated aspartate aminotransferase (35%) and alanine aminotransferase (38%), decreased appetite (23%), alopecia (23%), and sensory neuropathy (23%). These events were consistent with known toxicity profiles of antibody-drug conjugates and gemcitabine, and were generally reversible with supportive management.
Expert Commentary
These results are compelling within a population that lacks access to cisplatin-based therapy. By targeting HER2-positive disease, DV combined with gemcitabine may represent a precision oncology approach that circumvents cisplatin-related contraindications. The high pCR rate observed in four-cycle recipients reinforces the need to consider regimen duration in future trial designs. Notably, pCR is a strong surrogate marker for long-term survival in MIBC, though confirmation in phase 3 trials is essential.
Limitations include the single-arm design, small sample size, and absence of a control group, which preclude definitive comparative efficacy conclusions. Potential HER2 testing variability across centers may also influence patient selection accuracy. However, the multicenter nature enhances external validity and supports further trials.
Biologically, DV’s mechanism—internalization of the HER2-antibody complex followed by intracellular release of a cytotoxic payload—offers rationale for enhanced tumor cell kill. The combination with gemcitabine, a nucleoside analog inhibiting DNA synthesis, may provide additive or synergistic effects.
Conclusion
Disitamab Vedotin plus gemcitabine demonstrates promising efficacy and manageable safety as neoadjuvant therapy for HER2-positive MIBC patients unsuitable for cisplatin. Four treatment cycles may yield superior responses compared to three cycles. While these findings suggest a potential shift in preoperative management, randomized controlled trials are needed to validate survival benefit, identify optimal HER2 selection criteria, and assess long-term tolerability.
Funding and Clinical Trial Registration
This research was conducted under multicenter protocols. Clinical trial registration details were not specified in the provided summary. The trial findings have been published in Eur Urol, with DOI: 10.1016/j.eururo.2025.10.009.
References
Huang H, Ma W, Zeng X, Liu B, Dai H, Zhou G, Wan J, Zhang Y, Hu Z, Yang C. Efficacy and Safety of Disitamab Vedotin Combined with Gemcitabine as Neoadjuvant Therapy in Muscle-invasive Bladder Cancer: An Open-label, Multicenter, Single-arm, Phase 2 Trial. Eur Urol. 2025 Nov 4:S0302-2838(25)04768-2. doi: 10.1016/j.eururo.2025.10.009. PMID: 41193372.