Highlights
- Deferoxamine (DFO) treatment was associated with a twofold higher odds of early neurological improvement (EMNI) within the first week of intracerebral hemorrhage (ICH).
- The therapeutic effect of DFO appears most pronounced in patients with moderate hematoma volumes (10–30 mL), showing significant functional benefits at 180 days.
- Recovery in ICH patients continues well beyond the standard 90-day assessment window; DFO may favorably alter the recovery trajectory between 3 and 6 months.
- Perihematomal edema (PHE) becomes increasingly hypodense on CT over time, but these radiological changes do not necessarily correlate with long-term clinical outcomes.
Background: The Iron Toxicity Hypothesis in ICH
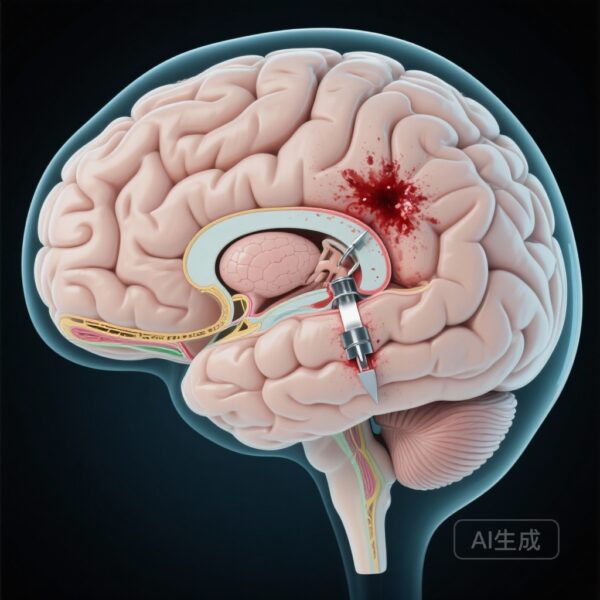
Spontaneous intracerebral hemorrhage (ICH) remains one of the most devastating forms of stroke, characterized by high mortality and profound long-term disability. Beyond the initial mechanical injury caused by the hematoma, secondary brain injury (SBI) plays a critical role in determining patient outcomes. A primary driver of SBI is the degradation of hemoglobin and the subsequent release of free iron into the perihematomal tissue. This iron overload triggers oxidative stress, inflammation, and neuronal apoptosis.
Deferoxamine mesylate, an FDA-approved iron chelator, has shown promise in preclinical models by reducing iron-mediated neurotoxicity and perihematomal edema. However, translating these findings into clinical success has proven challenging. The Intracerebral Hemorrhage Deferoxamine (i-DEF) trial was designed to evaluate the safety and potential efficacy of this intervention, and recent secondary analyses have provided nuanced insights into which patients might benefit most and how we should measure success in future ICH trials.
Study Design: The i-DEF Trial
The i-DEF trial (NCT02175225) was a multicenter, randomized, placebo-controlled, double-blind, phase 2 trial utilizing a futility design. The study enrolled 294 adults (aged 18–80) with primary, spontaneous, supratentorial ICH across 40 hospitals in Canada and the USA. Participants were randomized 1:1 to receive either deferoxamine mesylate (32 mg/kg per day) or a saline placebo via infusion for three consecutive days, initiated within 24 hours of symptom onset.
The primary outcome was a “good clinical outcome,” defined as a modified Rankin Scale (mRS) score of 0–2 at day 90. The futility analysis was prespecified: if the 90% upper confidence bound of the absolute risk difference between groups was less than 12% in favor of deferoxamine, further phase 3 testing would be considered futile.
Key Findings and Post Hoc Insights
1. Primary Results and Safety
The initial findings, published in Lancet Neurology, indicated that deferoxamine was safe and well-tolerated. However, at day 90, 34% of the deferoxamine group achieved an mRS of 0–2 compared to 33% in the placebo group. The adjusted absolute risk difference was only 0.6%, leading to the conclusion that a phase 3 trial for an unselected ICH population would be futile based on the 90-day primary endpoint. Despite this, the safety profile was encouraging, with no significant difference in serious adverse events or mortality between the groups.
2. Early Neurological Improvement (EMNI)
A post hoc analysis focusing on the first week of treatment revealed a different perspective. Researchers evaluated EMNI, defined as a decrease in the National Institutes of Health Stroke Scale (NIHSS) score of 4 or more points from baseline. Deferoxamine was associated with a twofold higher odds of EMNI (OR 2.30; 95% CI 1.07–4.95). Importantly, EMNI was a strong predictor of favorable outcomes at 90 and 180 days, suggesting that DFO exerts a biological effect much earlier than previously captured by standard endpoints.
3. The Influence of Hematoma Volume
One of the most significant findings from the post hoc data relates to hematoma volume (HV). When participants were stratified into small (<10 mL), moderate (10–30 mL), and large (>30 mL) volumes, a clear differential treatment effect emerged. Patients with moderate HV treated with deferoxamine had significantly higher odds of a favorable outcome at 180 days (50% vs. 25.5%; aOR 2.7). This suggests a “therapeutic window” where the iron-chelating effect is sufficient to mitigate damage in moderate bleeds but may be overwhelmed by large bleeds or unnecessary in very small ones.
4. Shifting the Recovery Timeline
Traditional stroke trials focus on 90-day outcomes, but the i-DEF data suggests this may be insufficient for ICH. Analysis of the recovery trajectory showed that the proportion of patients with mRS 0–2 continued to increase up to 180 days in both groups. However, the deferoxamine group showed a statistically significant improvement between day 90 and day 180, while the placebo group plateaued. This indicates that deferoxamine may not just protect the brain acutely but also facilitate a more robust long-term recovery process.
5. Radiological Markers: Perihematomal Edema
The trial also examined the evolution of perihematomal edema (PHE) using CT scans. While the mean Hounsfield Units (mHU) of PHE decreased significantly from baseline to day 3–4 (becoming more hypodense), this change did not correlate with clinical outcomes at 90 or 180 days. This finding challenges the utility of PHE hypodensity as a primary radiological surrogate marker in ICH research, suggesting that the volume of edema or other physiological factors may be more relevant than its radiodensity.
Expert Commentary and Clinical Implications
The i-DEF trial results highlight a common pitfall in neuroprotection research: the use of overly broad inclusion criteria and short-term primary endpoints. While the trial met its futility criteria for the general ICH population at 90 days, the post hoc analyses provide a compelling argument for a more targeted approach.
The data regarding moderate hematoma volumes and the extended recovery trajectory are particularly practice-changing. Clinicians should be aware that ICH recovery is a marathon, not a sprint, and that therapeutic interventions may show their true value months after the initial event. Furthermore, the EMNI data suggests that DFO does have a measurable impact on neurological status during the acute phase, even if it doesn’t immediately translate to mRS shifts for every patient.
Future trials should consider:
- Enriching study populations with patients having moderate hematoma volumes (10–30 mL).
- Extending primary outcome assessments to 180 days or even one year.
- Utilizing NIHSS-based early improvement markers as secondary or intermediate endpoints.
Conclusion
In summary, while deferoxamine did not meet the threshold for a general phase 3 trial in ICH, the i-DEF program has yielded invaluable data on the nature of ICH recovery. Deferoxamine appears to double the odds of early neurological improvement and significantly benefits those with moderate-sized hemorrhages over a 6-month period. These findings provide a roadmap for future neuroprotective strategies, emphasizing the need for patient stratification and longer-term follow-up in clinical trial design.
Funding and Registration
The i-DEF trial was funded by the US National Institutes of Health (NIH) and the National Institute of Neurological Disorders and Stroke (NINDS). ClinicalTrials.gov Identifier: NCT02175225.
References
- Polymeris AA, et al. Evolution of Perihematomal Edema Mean Hounsfield Unit and Its Association with Clinical Outcome in Intracerebral Hemorrhage: A Post Hoc Analysis of the i-DEF Trial. Neurocrit Care. 2025.
- Polymeris AA, et al. Early neurological improvement with deferoxamine after intracerebral hemorrhage: A post hoc analysis of the i-DEF trial. Int J Stroke. 2025.
- Selim M, et al. Deferoxamine mesylate in patients with intracerebral haemorrhage (i-DEF): a multicentre, randomised, placebo-controlled, double-blind phase 2 trial. Lancet Neurol. 2019.
- Foster L, et al. Effect of Deferoxamine on Trajectory of Recovery After Intracerebral Hemorrhage: A Post Hoc Analysis of the i-DEF Trial. Stroke. 2022.
- Wei C, et al. Effect of Deferoxamine on Outcome According to Baseline Hematoma Volume: A Post Hoc Analysis of the i-DEF Trial. Stroke. 2022.