Highlight
The phase 3 TROPION-Breast01 study represents a pivotal moment in the management of hormone receptor-positive, HER2-negative (HR+/HER2-) metastatic breast cancer. Key highlights include:
- A statistically significant and clinically meaningful improvement in progression-free survival (PFS) with datopotamab deruxtecan (Dato-DXd) compared to investigator’s choice of chemotherapy (ICC).
- A primary PFS hazard ratio (HR) of 0.63, representing a 37% reduction in the risk of progression or death.
- The final overall survival (OS) analysis yielded a hazard ratio of 1.01, likely influenced by a high rate of subsequent antibody-drug conjugate (ADC) therapy in the control arm.
- A significantly lower incidence of grade 3 or higher treatment-related adverse events (TRAEs) with Dato-DXd (20.8%) compared to ICC (44.7%).
Background and Disease Burden
Hormone receptor-positive, HER2-negative (HR+/HER2-) breast cancer is the most common subtype of breast cancer worldwide. While endocrine therapy combined with CDK4/6 inhibitors remains the first-line standard of care for metastatic disease, nearly all patients eventually develop endocrine resistance. Once resistance occurs, treatment options often transition to sequential single-agent chemotherapy. However, traditional cytotoxic agents are associated with limited durability of response and significant cumulative toxicity, including myelosuppression and neuropathy.
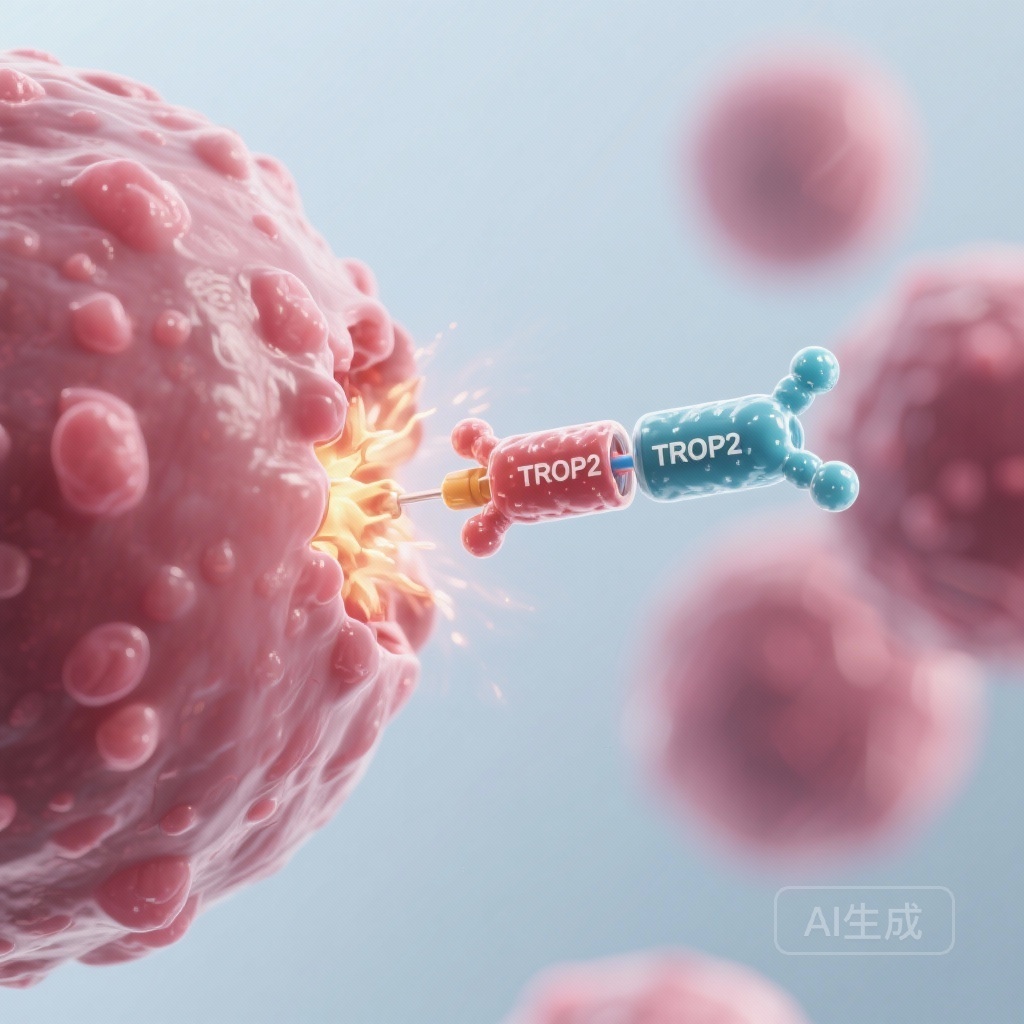
Trophoblast cell-surface antigen 2 (TROP2) is a transmembrane glycoprotein overexpressed in the majority of breast cancers, regardless of subtype, making it an attractive target for antibody-drug conjugates (ADCs). Datopotamab deruxtecan (Dato-DXd) is a TROP2-directed ADC consisting of a humanized anti-TROP2 IgG1 monoclonal antibody linked to a topoisomerase I inhibitor payload (a deruxtecan derivative) via a tetrapeptide-based cleavable linker. The TROPION-Breast01 trial was designed to evaluate whether Dato-DXd could provide a more effective and less toxic alternative to standard chemotherapy in the late-line setting.
Study Design
TROPION-Breast01 (NCT05104866) is a global, randomized, open-label, phase 3 study. The trial enrolled 732 adult patients with inoperable or metastatic HR+/HER2‒ breast cancer. Eligible patients must have experienced disease progression on endocrine therapy (or were deemed unsuitable for further endocrine therapy) and had received one to two prior lines of chemotherapy in the metastatic setting.
Participants were randomized 1:1 to receive either:
- Datopotamab deruxtecan: 6 mg/kg administered intravenously once every three weeks.
- Investigator’s Choice of Chemotherapy (ICC): Eribulin, vinorelbine, capecitabine, or gemcitabine.
The dual primary endpoints were PFS as assessed by blinded independent central review (BICR) and overall survival (OS). Secondary endpoints included investigator-assessed PFS, objective response rate (ORR), duration of response (DOR), and safety profiles.
Key Findings: Progression-Free and Overall Survival
Efficacy Outcomes
In the primary analysis, Dato-DXd demonstrated a superior PFS compared to ICC. The median PFS by BICR was 6.9 months for the Dato-DXd group versus 4.9 months for the ICC group (HR 0.63; 95% CI, 0.52 to 0.76; P < .0001). This benefit was consistent across all pre-specified subgroups, including patients with varying levels of TROP2 expression and those with or without prior CDK4/6 inhibitor treatment.
At the final OS analysis, with a median follow-up of 22.8 months, the results showed a median OS of 22.8 months for Dato-DXd and 20.6 months for ICC. However, the hazard ratio was 1.01 (95% CI, 0.83-1.22; P = 0.9445), failing to reach statistical significance. Researchers noted a significant imbalance in subsequent therapies; specifically, 24.0% of patients in the ICC arm received a subsequent ADC (such as trastuzumab deruxtecan or sacituzumab govitecan) compared to only 12.3% in the Dato-DXd arm. This crossover likely diluted the potential OS benefit of Dato-DXd.
Secondary Endpoints and Response Quality
Despite the neutral OS, secondary endpoints consistently favored Dato-DXd. The objective response rate (ORR) was significantly higher in the Dato-DXd arm (36.4%) compared to the ICC arm (22.5%). Furthermore, the time to first subsequent therapy (TFST) was longer for patients receiving Dato-DXd, suggesting a more durable period of clinical benefit before needing to switch to a different treatment modality.
Safety and Tolerability
One of the most compelling aspects of the TROPION-Breast01 data is the safety profile. Treatment-related adverse events (TRAEs) of grade 3 or higher occurred in 20.8% of the Dato-DXd group, which was less than half the rate seen in the ICC group (44.7%).
The most common toxicities for Dato-DXd were nausea (51.1%) and stomatitis (50.0%), though these were predominantly grade 1 or 2. In contrast, the ICC arm was characterized by higher rates of hematologic toxicity, particularly neutropenia (42.5%, with 30.8% being grade 3 or higher). Interstitial lung disease (ILD), a known risk with deruxtecan-based ADCs, was reported in 3.3% of patients in the Dato-DXd arm, mostly low-grade, with only one grade 3 event and no grade 4 or 5 events.
Expert Commentary
The interpretation of TROPION-Breast01 requires a nuanced understanding of the current metastatic breast cancer landscape. While the lack of OS benefit might initially seem disappointing, clinical experts emphasize that in the modern era of oncology, OS is increasingly difficult to prove in later lines of therapy due to the availability of effective subsequent treatments. The fact that twice as many patients in the control arm received a subsequent ADC suggests that the control group’s survival was significantly bolstered by these potent agents.
Mechanistically, Dato-DXd utilizes a stable linker and a potent topoisomerase I inhibitor, which allows for a high drug-to-antibody ratio while maintaining a favorable safety profile. The lower rate of severe neutropenia compared to traditional chemotherapy is a significant advantage for patient quality of life and treatment persistence. The primary takeaway for clinicians is that Dato-DXd offers a robust alternative that delays disease progression and reduces the toxicity burden compared to conventional chemotherapy in patients who have already exhausted endocrine options.
Conclusion
TROPION-Breast01 successfully met its primary endpoint of PFS, establishing datopotamab deruxtecan as a clinically meaningful advancement for patients with HR+/HER2- metastatic breast cancer. Although the final OS analysis did not show a statistically significant difference—confounded by the use of subsequent ADCs—the totality of the data supports Dato-DXd as a new standard-of-care option. Its superior efficacy over ICC, combined with a more manageable safety profile, addresses a critical unmet need for effective, less toxic therapies in the post-endocrine therapy setting.
Funding and Trial Information
The TROPION-Breast01 study was funded by AstraZeneca and Daiichi Sankyo. Detailed information regarding the trial can be found at ClinicalTrials.gov under the identifier NCT05104866.
References
1. Pistilli B, Jhaveri K, Im SA, et al. Datopotamab deruxtecan versus chemotherapy in previously treated inoperable/metastatic hormone-receptor-positive HER2-negative breast cancer: final overall survival analysis of the phase 3 TROPION-Breast01 study. Ann Oncol. 2025;S0923-7534(25)06337-9. doi:10.1016/j.annonc.2025.12.017.
2. Bardia A, Jhaveri K, Im SA, et al. Datopotamab Deruxtecan Versus Chemotherapy in Previously Treated Inoperable/Metastatic Hormone Receptor-Positive Human Epidermal Growth Factor Receptor 2-Negative Breast Cancer: Primary Results From TROPION-Breast01. J Clin Oncol. 2025;43(3):285-296. doi:10.1200/JCO.24.00920.