Highlight
– In 24,791 asymptomatic adults aged 50–64, CCTA-derived plaque extent and noncalcified atherosclerosis were independently associated with first coronary events over a median 7.8-year follow-up.
– Adding CCTA data to a model containing the pooled cohort equation (PCE) and coronary artery calcium score (CACS) improved discrimination (C statistic 0.764 → 0.779; P = .004) and yielded a net reclassification improvement (NRI) of 0.133.
– Reclassification mainly affected participants labeled low risk by PCE/CACS; CCTA modestly increased upward reclassification of those who later experienced events but also led to some over-classification in people who did not.
Background
Primary prevention of coronary heart disease hinges on accurate risk stratification to guide interventions such as lifestyle modification and lipid-lowering therapy. The pooled cohort equations (PCE) are widely used to estimate 10-year atherosclerotic cardiovascular disease risk and drive guideline-recommended treatment thresholds. Coronary artery calcium scoring (CACS) is now a well-established imaging biomarker used to refine risk, particularly in intermediate-risk individuals—CAC=0 downgrades risk, whereas high CAC supports initiation of statins.
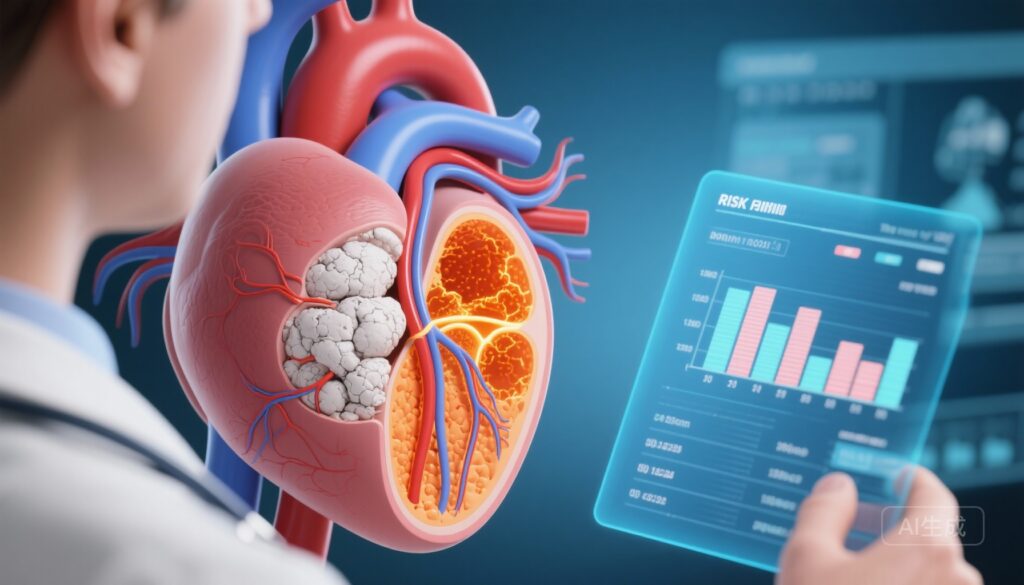
Despite these tools, many coronary events occur in people predicted to be at low to intermediate risk. Coronary computed tomography angiography (CCTA) provides more detailed anatomic information than CACS, detecting noncalcified plaque, nonobstructive plaque burden and obstructive disease. Whether that richer plaque characterization meaningfully improves primary prevention risk prediction beyond PCE and CACS has not been definitively established in a large, population-based cohort.
Study design
This observational cohort study (Bergström et al., JAMA 2025) prospectively enrolled 30,154 randomly recruited individuals aged 50–64 from the general population across six Swedish university hospitals (2013–2018). After exclusions for prior cardiovascular disease and low-quality imaging, 24,791 participants with high-quality CCTA images were analyzed. Baseline evaluation included cardiopulmonary imaging, physical examination, labs and questionnaires; national registers provided complete event follow-up through September 2024 (median follow-up 7.8 years).
Key exposures from CCTA were the segment involvement score (SIS, an index of the number of coronary segments with atherosclerotic plaque), presence of noncalcified plaque, and presence of obstructive coronary disease (≥50% stenosis). The primary outcome was first occurrence of nonfatal myocardial infarction or death from coronary heart disease.
Key findings
Among 24,791 participants, there were 304 coronary events during follow-up. Major results were:
- Extent of disease: Compared with participants with lower SIS, those with SIS 3–4 had a hazard ratio (HR) of 2.71 (95% CI, 1.34–5.44) and SIS >4 an HR of 5.27 (95% CI, 2.50–11.07) for the primary outcome.
- Noncalcified atherosclerosis: Presence of noncalcified plaque conferred an HR of 1.66 (95% CI, 1.23–2.22).
- Obstructive disease: The presence of stenosis ≥50% was associated with increased event risk (specific HRs reported in the article), consistent with the greater prognostic weight of anatomically severe disease.
When CCTA-derived data were added to a model containing PCE and CACS, model performance improved:
- C statistic (discrimination) improved from 0.764 to 0.779 (P = .004).
- Net reclassification improvement (NRI) was 0.133 (95% CI, 0.031–0.165), with a net correct upward reclassification of 14.2% among those who experienced events and incorrect upward classification of 1.6% among those who did not.
- Because overall event rates were low, most reclassification occurred among participants initially categorized as low risk (<5% 10-year PCE risk).
Clinical interpretation of effect sizes
The SIS results show a graded relationship between anatomic plaque extent and event risk: even modest segmental involvement (3–4 segments) approximately doubled to tripled risk, and more extensive involvement (>4 segments) increased risk fivefold. The independent association of noncalcified plaque is important because these lesions may be missed by CACS (which detects only calcified plaque) and are considered more vulnerable from a pathobiologic standpoint.
Net clinical impact
The statistical improvements in discrimination and reclassification were modest in absolute terms. Importantly, the improvement aligns with a plausible clinical niche: identifying a subset of patients labeled low risk by traditional tools who nonetheless harbor anatomically significant, noncalcified or more extensive atherosclerosis. In practice, this could change preventive management (for example, initiation of statin therapy) for a minority of individuals, but would also expose some people without events to intensified therapy or further testing.
Expert commentary and context
These findings add to a growing literature on the potential role of anatomic coronary imaging in prevention. Randomized trials in symptomatic populations have shown that CCTA can improve diagnostic certainty and downstream outcomes (for example, SCOT-HEART and PROMISE in patients with chest pain), and observational cohorts such as MESA demonstrated the strong prognostic value of CACS in asymptomatic individuals.
Guidelines currently endorse CACS as a primary imaging tool to refine decision-making for primary prevention in select intermediate-risk patients (for example, when statin decision is uncertain). By contrast, routine CCTA for asymptomatic screening is not recommended because of concerns about radiation exposure, cost, incidental findings, and uncertain net benefit. The present study suggests CCTA can detect clinically relevant plaque missed by CACS and may modestly improve risk models, but whether this translates into better patient-centered outcomes (reduced MI or death) when used to guide preventive therapy remains unproven.
Limitations
- Observational design: Associations do not prove that CCTA-guided management will reduce events. Downstream management after CCTA (statin initiation, revascularization) could confound observed associations.
- Population generalizability: The cohort was Swedish adults aged 50–64; results may not extrapolate to younger or older groups or to populations with different ethnic or socioeconomic characteristics.
- Event rate and clinical magnitude: With only 304 events, improvements in discrimination were statistically significant but modest; the absolute number of reclassified people who benefit is small.
- Resource and harm considerations: CCTA involves ionizing radiation, intravenous contrast, potential incidental findings prompting further testing, and higher cost than CAC scanning. These factors limit broad screening applicability.
Practical implications for clinicians
At present, CCTA should not replace PCE or CACS as a routine screening tool in asymptomatic populations. However, clinicians may consider CCTA selectively in carefully chosen situations, such as:
- Individuals with low PCE and zero CAC but persistent clinical concern (family history, atypical yet persistent symptoms) where detection of noncalcified plaque would materially change management.
- Cases where a more complete anatomic assessment (extent of nonobstructive plaque or unexpected obstructive disease) would alter preventive therapy or trigger further diagnostic testing.
Shared decision-making should weigh potential benefits (reclassifying hidden high-risk anatomy) against harms (radiation, contrast, downstream procedures, psychological impact, and cost). For most primary prevention decisions, CACS remains the preferred first-line imaging adjunct to clinical risk scores.
Research and policy gaps
Key next steps include:
- Randomized controlled trials to test whether CCTA-guided preventive strategies (e.g., statin initiation/intensification, aggressive risk factor management) reduce hard outcomes compared with standard care guided by PCE and CACS.
- Cost-effectiveness analyses comparing a strategy of selective CCTA versus CACS-first algorithms in different risk strata and healthcare systems.
- Subgroup analyses across age, sex, and racial/ethnic groups to define populations most likely to benefit.
- Studies quantifying downstream testing, revascularization, and adverse effects from a CCTA-first prevention strategy.
Conclusion
In this large, population-based cohort, CCTA-derived measures of coronary atherosclerosis—particularly plaque extent and the presence of noncalcified lesions—were independently associated with first coronary events and modestly improved risk prediction beyond the PCE and CACS. The improvement was statistically significant but modest in absolute terms, and reclassification mainly affected people originally classified as low risk. While CCTA can uncover clinically meaningful anatomic disease missed by calcium scoring, routine use for primary prevention is not yet supported. Selective use in carefully chosen cases and prospective trials assessing outcome benefits are warranted before broad implementation.
Funding and clinicaltrials.gov
Funding sources and trial registration details are reported in the original JAMA publication (Bergström et al., 2025).
References
1. Bergström G, Engström G, Björnson E, et al. Coronary Computed Tomography Angiography in Prediction of First Coronary Events. JAMA. 2025 Nov 9. doi:10.1001/jama.2025.21077.
2. Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk. Circulation. 2014;129(25 Suppl 2):S49–S73.
3. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC Guideline on the Management of Blood Cholesterol. Circulation. 2019;139(25):e1082–e1143.
AI-friendly thumbnail prompt
A high-resolution, photorealistic scene in a modern clinical setting: a middle-aged adult (50–64 years) sits at a desk reviewing a tablet showing a coronary CT angiogram; the screen displays coronary arteries with both white calcified spots and orange noncalcified plaque, while a clinician points at a highlighted stenosis; subdued clinical background, neutral color palette, clear focus on the CT image and the shared patient-clinician interaction.