Highlights
- Equitable access to minimally invasive surgical (MIS) resection for colon cancer could reduce total hospital stays by thousands of days across the health system.
- Patients aged 65 and older, those with frailty or comorbidities, and individuals from socioeconomically deprived areas are significantly less likely to receive MIS.
- Correcting these disparities is associated with a reduction in 1-year mortality and a substantial decrease in 30-day readmission rates.
- The study highlights a critical need for targeted interventions to ensure that surgical innovation benefits all patient demographics equally.
Introduction: The Promise of Minimally Invasive Surgery
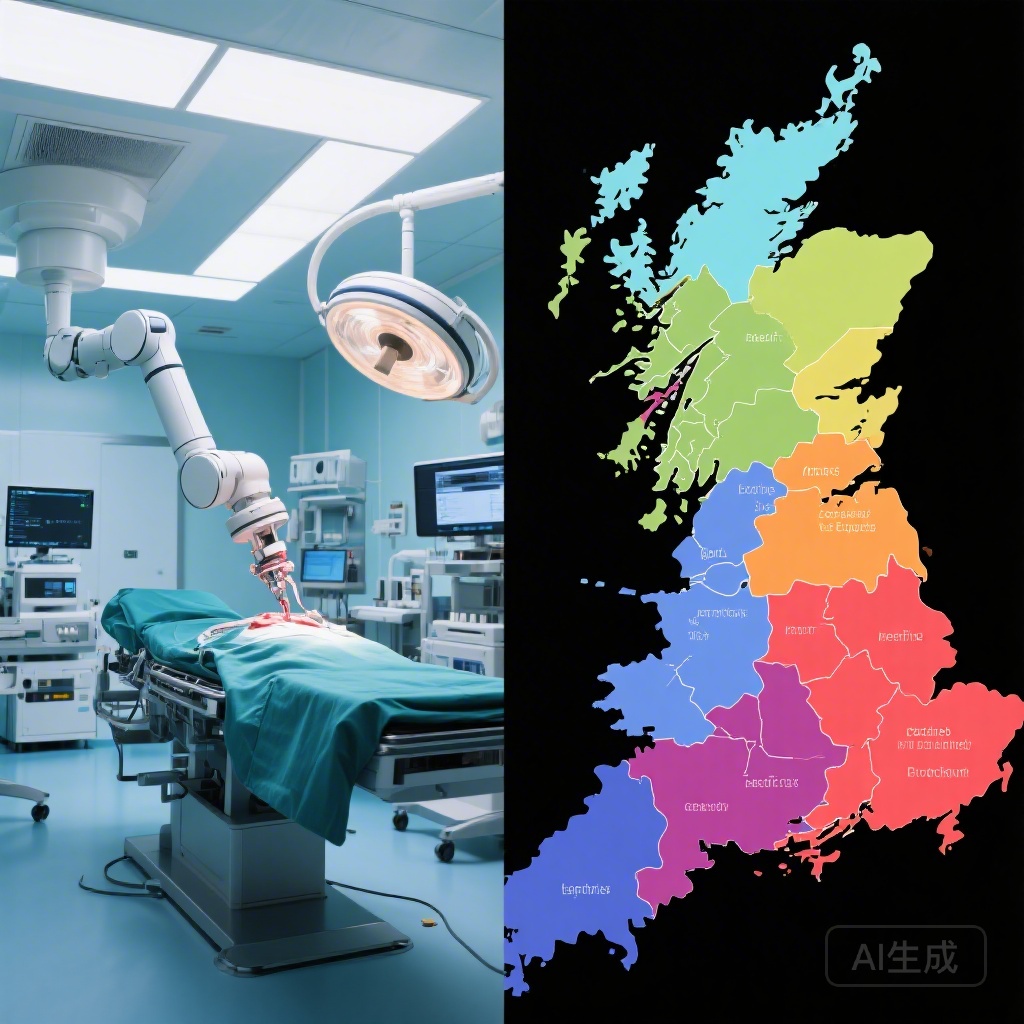
Minimally invasive surgical (MIS) resection, including laparoscopic and robotic-assisted techniques, has revolutionized the elective management of colon cancer. Compared to traditional open surgical resection, MIS is associated with reduced intraoperative blood loss, faster recovery of bowel function, and shorter hospital stays without compromising oncological outcomes. Despite these well-documented advantages and the inclusion of MIS in standard clinical guidelines, its uptake is not uniform across the population.
Historically, surgical innovation often trickles down through the most advantaged patient groups first. In the context of colon cancer, anecdotal and preliminary data have long suggested that older patients or those with complex medical backgrounds are frequently funneled toward open surgery due to perceived risks or technical challenges. This population-based study, published in The Lancet Oncology, provides a rigorous estimation of the potential benefits that could be realized if these systemic inequalities in MIS access were corrected.
The Burden of Inequality in Surgical Care
Health inequalities in England remain a significant challenge for the National Health Service (NHS). While the overall survival for colon cancer has improved, the gap between the most and least deprived individuals, and between younger and older patients, persists. The decision to perform MIS versus open surgery is often multifactorial, involving surgeon expertise, hospital resources, and patient-specific factors. However, when clinical decisions are influenced by socioeconomic status or age-related bias rather than purely physiological fitness, the healthcare system fails to deliver equitable care.
The burden of these inequalities is twofold: first, the individual patient suffers a more invasive procedure with a longer recovery time; second, the healthcare system incurs higher costs and resource utilization due to extended hospital stays and higher complication rates associated with open surgery.
Study Design and Methodology
This population-based study analyzed data from 10,603 adult patients (aged 15–99 years) diagnosed with stage I–III colon carcinoma in England between January and December 2022. To ensure a focus on elective, curative-intent care, the researchers excluded patients diagnosed through emergency routes, those with metastatic disease (stage IV), and those treated in private hospitals or low-volume NHS Trusts (ten or fewer resections per year).
The researchers utilized a potential outcomes framework to model scenarios where inequalities in MIS uptake were corrected within each NHS Trust. They specifically targeted four “suboptimal uptake groups”:
- Patients aged 65 years and older.
- Patients with existing frailty (moderate or high frailty scores).
- Patients with multiple comorbidities.
- Patients living in the most socioeconomically deprived quintiles.
The primary outcomes measured included the length of index hospital stay, total hospital stay, the probability of readmission within 30 days, and 1-year mortality. By contrasting observed outcomes with these hypothetical “corrected” scenarios, the study estimated the systemic impact of achieving surgical equity.
Key Findings: Quantifying the Benefits of Equity
The study cohort consisted of 5,487 (51.7%) males and 5,116 (48.3%) females, with a mean age of 70.3 years. MIS was attempted in 84.0% of cases and successfully completed in 75.0%. However, the disparities among the target groups were stark.
Disparities in MIS Uptake
The data confirmed significant gaps in the use of MIS:
- Age: 73.8% in those 65+ vs. 77.8% in those under 65.
- Deprivation: 73.9% in the most deprived quintiles vs. 76.2% in the least deprived.
- Comorbidity: 70.8% in those with comorbidities vs. 76.9% in those without.
- Frailty: 64.1% in patients with moderate/high frailty vs. 76.2% in those with low frailty scores.
Impact on Hospital Resource Utilization
The benefits of MIS were most visible in hospital stay durations. Patients undergoing MIS had hospital stays that were 3 to 4 days shorter than those undergoing open surgery. When modeling the effect of correcting inequalities, the researchers found that total hospital stays could be reduced by:
- 1,567 days by correcting age-related inequality.
- 975 days by correcting deprivation-related inequality.
- 912 days by correcting comorbidity-related inequality.
- 682 days by correcting frailty-related inequality.
Clinical Outcomes and Survival
Beyond hospital efficiency, the clinical benefits were profound. The proportion of 30-day readmissions was significantly lower in the MIS group (13.1%) compared to the open surgery group (18.1%). Most importantly, 1-year mortality was more than 50% lower in patients receiving MIS (2.9%) compared to those receiving open surgery (7.9%). While some of this difference may be attributed to patient selection, the potential outcomes framework suggests that a significant portion of this survival benefit is directly linked to the surgical approach itself.
Expert Commentary: Navigating the Barriers to Implementation
The findings of this study present a compelling case for health policy experts and surgical leads. However, translating these findings into practice requires addressing the underlying reasons for these inequalities. Surgeons may be more hesitant to perform MIS on frail or elderly patients due to concerns about prolonged anesthesia or the physiological stress of pneumoperitoneum. Similarly, patients in deprived areas may present later or to hospitals with fewer resources for advanced robotic or laparoscopic platforms.
Expert clinicians suggest that “prehabilitation”—optimizing a patient’s physical and nutritional status before surgery—could be the key to making MIS a viable option for those currently deemed too frail or comorbid. Furthermore, there is a call for standardized training and resource allocation to ensure that every NHS Trust has the capability to offer MIS to all eligible patients, regardless of their background.
Critics might point out that the study’s observational nature makes it difficult to fully separate the benefits of the surgery from the baseline health of the patient (selection bias). Nevertheless, the magnitude of the reduction in hospital days and mortality suggests that even if only a fraction of the effect is causal, the impact on public health would be substantial.
Conclusion: A Call to Action for Health Systems
This population-based study underscores that MIS is not just a technical preference but a tool for health equity. Correcting the inequalities in its implementation has the potential to significantly reduce the burden of colon cancer on both the patient and the healthcare system. By reducing hospital stays and mortality, equitable access to MIS can help bridge the survival gap that has long plagued oncology care.
Moving forward, healthcare providers and policymakers must prioritize the expansion of MIS programs, specifically targeting those groups currently left behind. As we move toward a more data-driven healthcare model, addressing these disparities will be essential for achieving the goal of high-quality, equitable cancer care for all.
Funding and References
This study was funded by Cancer Research UK.
Reference:
Maringe C, O’Leary D, Benitez-Majano S, Leyrat C, Exarchakou A, Rachet B, Quaresma M. Estimated effect of correcting inequalities in minimally invasive surgical resection in patients with colon cancer in England: a population-based study. Lancet Oncol. 2026 Feb;27(2):212-222. doi: 10.1016/S1470-2045(25)00648-5. PMID: 41643697.