High-Level Highlights
- The SMARTEST trial is the first register-based randomized clinical trial (RRCT) to compare an SGLT2 inhibitor (dapagliflozin) directly against metformin as a first-line therapy in early-stage type 2 diabetes (T2D).
- Baseline analysis of 2,072 participants shows that even in the early stages of T2D (duration <4 years), there is a significant prevalence of hypertension (64.4%) and dyslipidemia (57.1%).
- Interim results revealed an unexpectedly high rate of microvascular complications (11.7 events per 100 patient-years), contrasting with relatively low rates of major adverse cardiovascular events (MACE) and death.
- The trial demonstrates the feasibility of a decentralized, register-based methodology in primary care, potentially setting a new standard for large-scale clinical research.
Introduction: The Metformin Paradigm Under Scrutiny
For decades, metformin has been the undisputed cornerstone of type 2 diabetes (T2D) management. Since the landmark UK Prospective Diabetes Study (UKPDS), it has been the preferred first-line agent due to its efficacy in glucose lowering, safety profile, and low cost. However, the landscape of diabetology has shifted dramatically over the last decade with the emergence of sodium-glucose cotransporter-2 (SGLT2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists. These newer classes have demonstrated profound cardiovascular and renal benefits that appear to be independent of their glucose-lowering effects.
While current guidelines from the ADA and EASD recommend SGLT2 inhibitors for patients with established cardiovascular or renal disease, their role as an initial therapy for patients with newly diagnosed, low-risk T2D remains a subject of intense debate. The SMARTEST trial (SGLT2 inhibitor or Metformin as standard treatment in early-stage type 2 diabetes) aims to provide the evidence needed to potentially challenge or reinforce the long-standing metformin-first paradigm.
Study Design: The Novel SMARTEST Methodology
The SMARTEST trial is a pioneering decentralized, register-based randomized clinical trial (RRCT). Unlike traditional clinical trials that rely on intensive, site-specific monitoring and manual data entry, the SMARTEST trial utilizes the Swedish National Diabetes Register (NDR) and the National Patient Register for automated data extraction. This approach allows for a more representative participant pool and significantly reduces the administrative burden on primary care centers.
The study included 2,072 participants diagnosed with T2D for less than four years. These individuals were randomized 1:1 to receive either dapagliflozin (10 mg/day) or an individualized dose of metformin. To reflect real-world clinical practice, the trial was open-label for participants and clinicians, but researchers remained blinded to endpoint data. The primary composite endpoint includes time to the first event of myocardial infarction, stroke, heart failure, progression of microvascular complications, or all-cause death.
Baseline Characteristics: A Real-World Snapshot
The baseline data from SMARTEST provides a sobering look at the health status of patients in the early stages of T2D. The mean age of the cohort was 61.2 years, with a balanced representation of the primary care population. Despite being early in their disease course, the participants exhibited a high burden of metabolic comorbidities:
- Hypertension: Present in 64.4% of the population.
- Dyslipidemia: Present in 57.1% of the population.
- Renal Health: Signs of nephropathy were already detectable in 6.1% of patients.
- Retinopathy: Found in 13.2% of the participants.
These figures emphasize that type 2 diabetes is rarely a solitary condition. Even at diagnosis, the vascular risk is already elevated, suggesting that the window for preventive intervention opens much earlier than previously thought.
Key Findings: The Unexpected Burden of Microvascular Disease
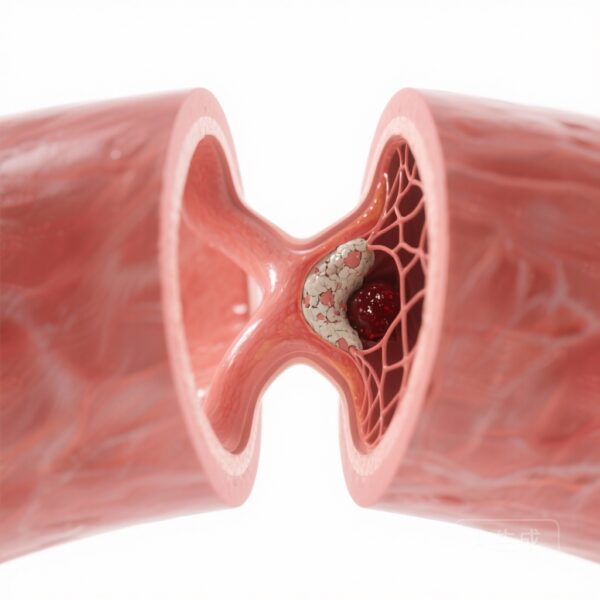
The blinded interim analysis, conducted at a mean follow-up of 19.0 months, yielded striking results. The overall event rate for the primary composite endpoint was 11.7 per 100 patient-years (py). While the rates of MACE (0.6/100 py) and all-cause death (0.3/100 py) were low—consistent with an early-stage, relatively healthy population—the rate of microvascular complications was unexpectedly high.
This high incidence of microvascular progression (including retinopathy and nephropathy) suggests that traditional management strategies may be insufficient in preventing the subtle, early damage caused by hyperglycemia and metabolic stress. If the final results of SMARTEST show that SGLT2 inhibitors can significantly reduce these early microvascular events compared to metformin, it could catalyze a major shift in how clinicians approach the first year of T2D diagnosis.
Expert Commentary: Mechanistic Insights and Clinical Implications
The biological plausibility for using SGLT2 inhibitors as a first-line agent is strong. Unlike metformin, which primarily works by reducing hepatic glucose production, SGLT2 inhibitors provide a multifaceted hemodynamic and metabolic benefit. By inducing glycosuria and natriuresis, they reduce blood pressure and intraglomerular pressure, offering direct nephroprotection. Furthermore, their effects on weight loss and uric acid reduction contribute to a more favorable cardiovascular profile.
However, the transition to SGLT2 inhibitors as a universal first-line therapy faces hurdles. Metformin is exceptionally cost-effective and has a long-term safety record spanning over 60 years. In many healthcare systems, the cost-benefit ratio will remain a critical factor. The SMARTEST trial will be essential in determining if the superior organ protection of SGLT2 inhibitors justifies the higher pharmaceutical expenditure in the primary care setting.
Conclusion: A Potential Paradigm Shift
The SMARTEST trial is more than just a comparison of two drugs; it is a test of our current philosophy of diabetes care. The high rate of microvascular events identified in the baseline and interim analysis serves as a call to action. We can no longer view “early-stage” diabetes as a low-risk period where conservative management is always sufficient.
As we await the final results in 2026, the feasibility of the RRCT model demonstrated here suggests that we can conduct large-scale, high-quality clinical research within the framework of routine primary care. Whether SMARTEST reinforces the metformin standard or establishes SGLT2 inhibitors as the new first-line therapy, it will undoubtedly provide the evidence needed to optimize the prevention of diabetic complications for millions of patients worldwide.
Funding and ClinicalTrials.gov
The SMARTEST trial is supported by grants from the Swedish Research Council, the Swedish Heart-Lung Foundation, and AstraZeneca (which provided dapagliflozin). The trial is registered at ClinicalTrials.gov (Identifier: NCT03982381) and EUDRA-CT (2019-001046-17).
References
- Eriksson JW, Fanni G, Lundqvist MH, et al. SGLT2 inhibitor or metformin as standard treatment in early-stage type 2 diabetes? Baseline data in SMARTEST, a novel, decentralised, register-based randomised trial on prevention of diabetic complications. Diabetes Obes Metab. 2026 Feb;28(2):1327-1338.
- Davies MJ, Aroda VR, Collins BS, et al. Management of hyperglycemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2022;65(12):1925-1966.
- Zelniker TA, Wiviott SD, Raz I, et al. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet. 2019;393(10166):31-39.