Introduction
Cancer remains a principal cause of morbidity and mortality in China, profoundly influenced by rapid demographic changes, industrialization, and lifestyle modifications. Recent decades have witnessed marked shifts in cancer epidemiology within the population, posing significant challenges and opportunities for national cancer control efforts. This article synthesizes current trends in cancer incidence, mortality, and survival in China, highlights key modifiable risk factors driving the disease burden, and elucidates governmental initiatives aimed at mitigating this public health threat.
Cancer Epidemiology in China
Cancer Incidence in 2022
In 2022, estimated new cancer cases numbered approximately 4.82 million, with a crude incidence rate of 341.75 per 100,000 persons. Distribution by sex revealed 2.53 million cases in males and 2.29 million in females. Lung cancer was the predominant diagnosis in both sexes, accounting for 22% of cases nationally, followed by colorectal (10.7%), thyroid (9.7%), liver (7.6%), stomach (7.4%), and female breast cancers (7.4%).
Sex-specific incidence data underscore distinct patterns: males exhibited higher lung (91.36/100,000), liver (37.16/100,000), stomach (34.20/100,000), and esophageal cancer rates (23.23/100,000), whereas females had markedly higher thyroid cancer incidence (49.40/100,000). Female breast cancer (51.71/100,000) and cervical cancer (21.81/100,000) also represent significant burdens.
Cancer Mortality in 2022
Cancer claimed an estimated 2.57 million deaths in 2022, corresponding to a crude mortality rate of 182.34 per 100,000. Males experienced a higher mortality burden (225.97/100,000) compared to females (136.79/100,000). Leading causes of death included lung (28.5%), liver (12.3%), stomach (10.1%), colorectal (9.3%), and esophageal cancers (7.3%).
Notably, lung cancer accounted for 31.7% of male and 23.0% of female cancer deaths. Major digestive system cancers presented higher mortality rates among males, while female sex-specific cancers, such as breast (10.86/100,000), cervical (8.06/100,000), and ovarian cancers (4.73/100,000), contribute significantly.
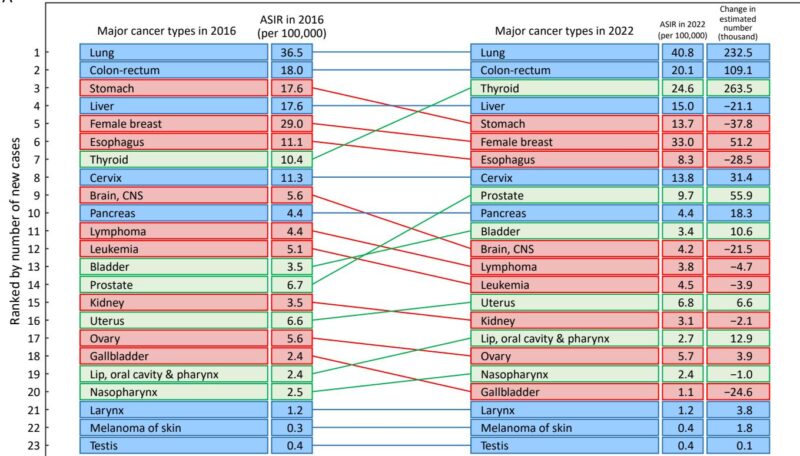
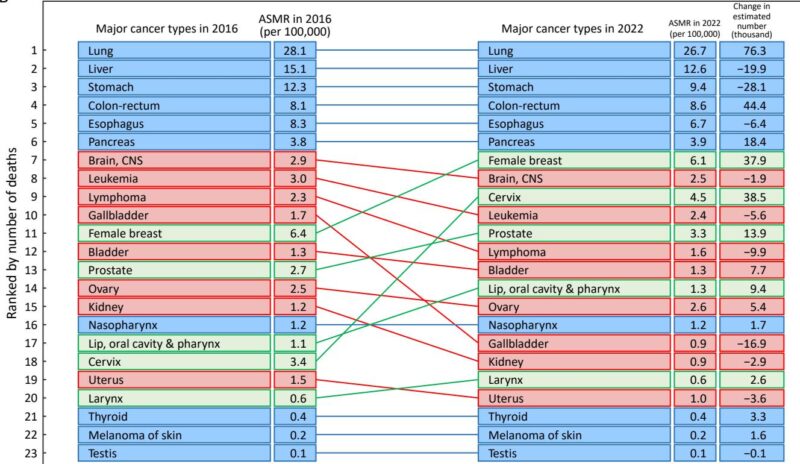
Temporal Trends and Rank Changes
From 2016 to 2022, lung and colorectal cancers maintained their positions as the most common malignancies, both with rising age-standardized incidence rates. Thyroid cancer incidence doubled, elevating its rank to third nationally. Prostate cancer incidence increased 1.5-fold, advancing to ninth in commonality.
Mortality rankings remained stable for lung, liver, stomach, colorectal, esophageal, and pancreatic cancers; however, sex-specific malignancies manifested upward mortality shifts. Female breast cancer rose from eleventh to seventh, and cervical cancer to ninth. Prostate cancer mortality also increased.
From 2000 to 2018, the age-standardized incidence rate (ASIR) for all cancers rose annually by approximately 1.4%, driven by notable female increases in thyroid and cervical cancers. Concurrently, the age-standardized mortality rate (ASMR) decreased annually by about 1.3%, reflecting improved outcomes.
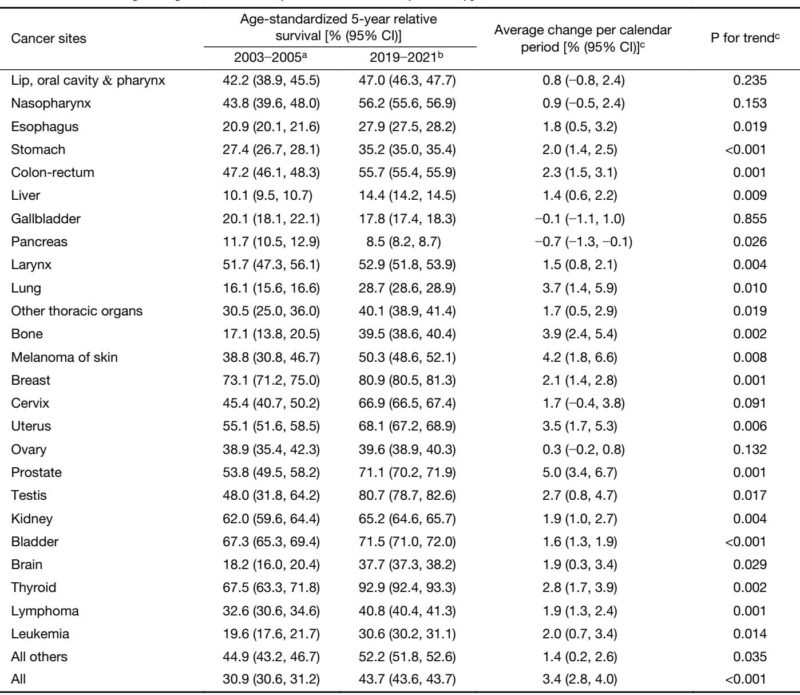
Survival Improvements
Five-year age-standardized relative survival for all cancers improved markedly from 30.9% in 2003–2005 to 43.7% in 2019–2021. Survival gains were observed across 19 cancer types, with prostate cancer showing the most pronounced improvement. Male patients exhibited lower overall survival compared to females (36.4% vs. 51.6%). Survival declines with advancing age were consistent across tumor types.
Cancers with favorable prognoses (>60% 5-year survival) included thyroid, breast, testicular, bladder, prostate, kidney, uterine, and cervical cancers. Poor survivals (<30%) were noted for pancreatic, liver, gallbladder, esophageal, and lung cancers.
Burden Attributable to Modifiable Risk Factors
Analysis of 2023 Global Burden of Disease data identified that modifiable risk factors accounted for nearly half of cancer deaths and disability-adjusted life years (DALYs). Approximately 49.9% of cancer deaths (1.28 million) were attributable to such factors, with higher impact among males (57.1%) than females (36.6%). Tobacco use was the leading contributor to cancer mortality and DALYs, particularly among males (44.9% and 42.6% respectively). Other significant risk factors included air pollution, dietary risks, high alcohol use, and unsafe sex.
National Cancer Prevention and Control Policies
Strategic Framework
China’s cancer control has evolved towards a comprehensive and institutionalized system. The Healthy China 2030 Plan (2016) and subsequent Medium- and Long-term Plan for Chronic Diseases (2017−2025) embedded cancer prevention as a national priority, emphasizing disease prevention, multidisciplinary collaboration, and life-course management.
The Healthy China Initiative (2019−2030) designated cancer control among 15 flagship programs, setting measurable targets for risk reduction, early detection, and clinical standards.
Implementation Plans
The 2019–2022 Implementation Plan for Cancer Prevention concretized goals for expanding screening, early diagnosis, and standard treatment protocols. Recent updates align with the Healthy China targets, aiming to increase 5-year survival to 46.6% by 2030 and improve risk factor control.
This shift reflects a transition from fragmented campaigns to integrated, long-term governance mechanisms promoting equitable and sustainable cancer prevention and care.
Comprehensive Prevention Policies
Programs such as China Healthy Lifestyle for All and National Demonstration Areas for Integrated Prevention have fostered behavioral risk reduction, health literacy, and early screening systems. The 2025 Healthy Weight Management campaign targets obesity, a key risk factor for several cancers.
Collectively, these represent system-wide, population-focused policies that address shared determinants across chronic diseases and cancer.
Primary Prevention Measures
Approximately 40% of cancers in China are preventable by targeting modifiable risks. Effective strategies include HPV vaccination programs, tobacco control policies, air pollution reduction, and public health education.
HPV Vaccination
HPV vaccination is pivotal in cervical cancer prevention. Despite WHO goals for 90% female coverage by 2030, China’s first-dose HPV vaccine coverage among adolescent girls remains low (~4% in 2022). Recent initiatives aim to expand free bivalent vaccine availability to schoolgirls, and national inclusion of HPV vaccination in the Immunization Program starting 2025 marks significant progress.
Tobacco Control
Tobacco use is the most impactful modifiable risk. China has ratified the WHO Framework Convention on Tobacco Control, implementing MPOWER measures such as advertising bans and smoke-free laws. Smoking prevalence has declined but remains high (23.2% overall; 43.9% in males). Despite legislative advances in major cities, nationwide smoke-free coverage reaches only 16.2% of the population, underscoring the need for enhanced enforcement and broader policy adoption.
Air Pollution
Fine particulate matter (PM2.5) constitutes a substantial carcinogen linked to lung cancer. Policies such as the 2013–2017 Air Pollution Prevention Plan have lowered ambient pollution levels in regions like Beijing, yet residual carcinogenic risks persist due to PM2.5 chemical constituents. Ongoing surveillance and component-specific pollution controls are imperative.
Health Education
Cancer literacy is recognized as a key modifiable determinant of prevention behavior and health outcomes. The Healthy China Initiative aims to bolster cancer knowledge awareness to 80% by 2030. Recent surveys report a national literacy rate of approximately 70%, though disparities exist. Enhanced education efforts, particularly among underserved populations, will facilitate adoption of preventive behaviors, screening uptake, and treatment adherence.
Secondary Prevention: Cancer Screening
Screening remains an essential strategy to reduce mortality through early detection. Organized population-based screening frameworks have been established since 2005, delivering free screening for major cancers across rural and urban areas. Extensive local programs supplement national efforts, tailored to regional cancer epidemiology.
Evidence-based screening interventions have demonstrated reductions in incidence and mortality: upper gastrointestinal endoscopy lowers cancer incidence by 23% and mortality by 57%; low-dose computed tomography reduces lung cancer mortality by 31%; colorectal cancer risk-adapted screening is cost-effective; liver cancer surveillance in hepatitis B carriers significantly improves survival; breast ultrasound outperforms mammography in high-risk women; and HPV testing enhances cervical cancer screening effectiveness.
National clinical guidelines for seven cancer types have standardized screening protocols, ensuring quality assurance, equitable access, and consistent follow-up. These policies underpin China’s transition toward uniform, high-quality cancer screening nationwide.
Opportunistic Screening
Recent policy supports expand opportunistic screening in clinical and health exam settings, effectuated via pilot projects for upper gastrointestinal cancers and urban programs involving major hospitals. Guidelines standardize cancer-related health check protocols to boost early detection consistency.
Conclusion
China’s coordinated cancer control policies and expanding screening efforts have yielded measurable declines in mortality and improved survival. Nevertheless, the aging population, industrial exposures, and lifestyle changes sustain significant challenges. Continued emphasis on modifiable risk factors, health literacy, and equitable screening access, coupled with investment in innovative research and multisectoral integration, is vital to further reduce China’s cancer burden and enhance population health outcomes.
References
The references are detailed in the original article: Cao W, Qin K, Liu B, Chen W. Cancer statistics in China: Epidemiology, risk factors, and prevention. Chin J Cancer Res. 2025;37(6):912-928. doi:10.21147/j.issn.1000-9604.2025.06.04 IF: 6.3 Q1 .