Highlights
– New preoperative basal calcitonin thresholds from a large multicenter cohort (N=509) correlate with the anatomical extent of lymph node metastasis in medullary thyroid carcinoma (MTC).
– Proposed cutoffs: 241.9 pg/mL for central compartment involvement; 693.9 pg/mL for ipsilateral lateral neck; 2378.5 pg/mL for bilateral/contralateral lateral neck; 2787.1 pg/mL for upper mediastinal metastasis.
– These thresholds (measured by electrochemiluminescence or chemiluminescence) outperformed American Thyroid Association (ATA) guideline thresholds in predicting lymph node metastasis and discriminating structural recurrence–free survival (SRFS) in both training and validation cohorts.
Background
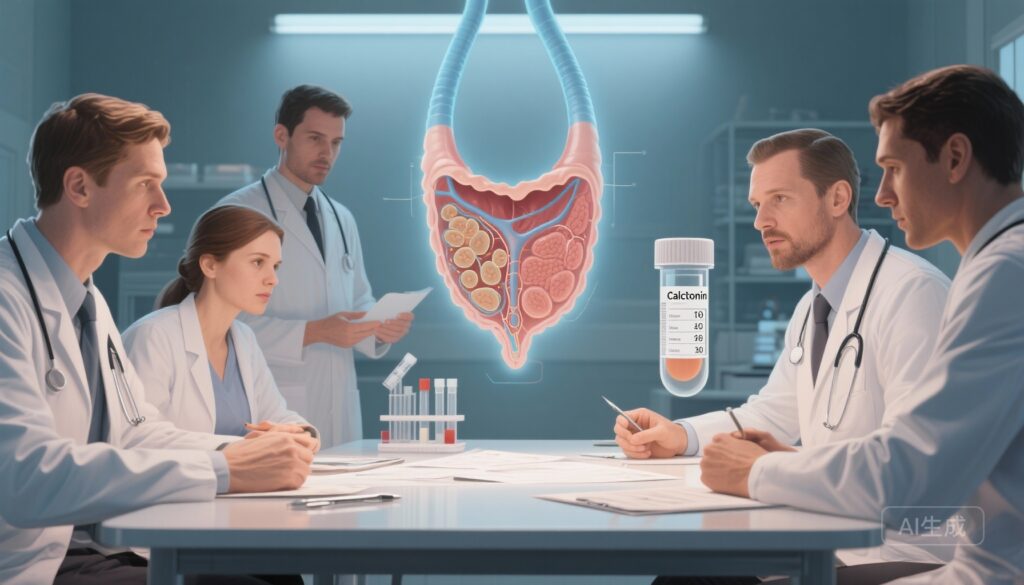
Medullary thyroid carcinoma (MTC) is a neuroendocrine tumor arising from parafollicular C cells and accounts for 3–5% of thyroid cancers. Calcitonin, produced by C cells, is the most sensitive and specific circulating biomarker for diagnosis, disease burden assessment, and postoperative surveillance in MTC. Accurate preoperative stratification of lymph node metastasis (LNM) is critical because the presence and extent of nodal disease determine the initial surgical approach — including the decision to perform prophylactic or therapeutic central and lateral neck dissections, and, less commonly, mediastinal dissection.
Study design
This retrospective multicenter cohort study (Chinese consortium of 13 hospitals; 2011–2024) included 509 patients with initially treated MTC who had preoperative basal calcitonin measured by contemporary immunoassays (electrochemiluminescence or chemiluminescence). Patients were randomly assigned 2:1 into training and validation cohorts. The main clinical outcome was structural recurrence–free survival (SRFS) stratified by calcitonin-derived groups. The investigators analyzed correlation between basal calcitonin and extent of LNM and used the training set to derive optimal thresholds for predicting location-specific nodal metastasis, then tested the thresholds in the validation set. Data were analyzed between June and September 2024.
Key findings
Patient characteristics and follow-up
Among 509 patients, median age was 50 years (IQR 40–59); 54.8% were female. Median follow-up was 52 months (IQR 27–84). Patients were categorized anatomically into four nodal groups: no LNM, central LNM, lateral LNM, and upper mediastinal LNM.
Correlation between basal calcitonin and LNM
There was a positive correlation between preoperative basal calcitonin and the extent of lymph node involvement (effect size η2 = 0.28), indicating a moderate-to-strong relationship between serum biomarker level and anatomical tumor spread.
Proposed calcitonin thresholds
Using the training cohort, investigators identified preoperative basal calcitonin thresholds associated with specific nodal patterns (assay units: pg/mL; note 1 pg/mL = 1 ng/L):
- 241.9 pg/mL — threshold associated with central compartment (level VI) LNM.
- 693.9 pg/mL — threshold associated with ipsilateral lateral neck LNM.
- 2787.1 pg/mL — threshold associated with upper mediastinal LNM.
- 2378.5 pg/mL — threshold associated with bilateral and/or contralateral lateral LNM.
These values were then tested in the validation cohort and retained predictive performance.
Comparative performance vs ATA guideline thresholds
Across both training and validation cohorts, the newly derived thresholds outperformed the cutoffs recommended in the American Thyroid Association (ATA) guideline in two respects: (1) they were more accurate in predicting the anatomical extent of LNM; and (2) they better discriminated SRFS, meaning they better stratified patients by risk of structural recurrence following initial treatment.
Clinical outcomes
Patients classified above the respective thresholds had higher rates of pathologically confirmed nodal metastasis in the corresponding compartments and worse SRFS compared with those below thresholds. The study supports use of assay-specific calcitonin cutoffs to predict nodal burden preoperatively and to tailor the anatomic extent of neck dissection.
Expert commentary and interpretation
These results update and refine the longstanding concept that basal calcitonin reflects tumor burden in MTC. The novelty here is calibration to modern immunoassays (electrochemiluminescence and chemiluminescence), which have largely replaced older platforms upon which previous thresholds and guideline recommendations were based. The study is large for a single histology with 509 patients, multicenter by design, and includes internal validation — strengths that increase confidence in the thresholds’ robustness.
Practical implications for surgeons and multidisciplinary teams
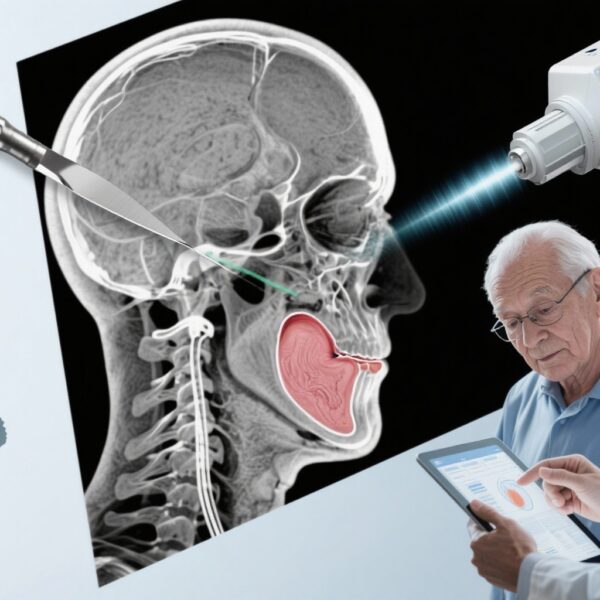
Surgeons planning initial management of MTC face a dilemma: undertreatment risks residual disease and early recurrence; overtreatment increases surgical morbidity (e.g., recurrent laryngeal nerve injury, hypoparathyroidism). Updated calcitonin thresholds tied to specific nodal compartments may permit more individualized decisions: for example, if basal calcitonin is <241.9 pg/mL and imaging does not show suspicious nodes, a more conservative approach to lateral neck dissection may be reasonable, while markedly elevated calcitonin levels above the lateral or mediastinal thresholds would raise the pretest probability sufficiently to justify more extensive compartment-oriented dissection even if cross-sectional imaging is equivocal.
Assay considerations and sex differences
Assay methodology matters. This study used contemporary electrochemiluminescence and chemiluminescence platforms; thresholds derived here should not be transposed indiscriminately to older or different assays without local cross-validation. The study abstract does not provide sex-stratified cutoffs; some prior literature suggests sex differences in baseline calcitonin, which could warrant sex-specific thresholds in future work.
Limitations and generalizability
Key limitations include retrospective design, potential inter-laboratory variability even among similar assay platforms, and the absence of prospective external validation outside the Chinese multicenter network. The cohort is geographically and ethnically specific; biological and care-delivery differences may affect generalizability. The study also does not replace individual anatomic imaging and clinical judgment; thresholds are an adjunct, not an absolute arbiter of surgical extent. Finally, the study used SRFS as the principal outcome but did not present long-term overall survival data, which in MTC can be influenced by mutation status (e.g., RET) and distant metastasis.
Clinical and research implications
For clinicians: consider incorporating assay-specific calcitonin thresholds into preoperative planning, while maintaining individualized assessment (high-resolution neck ultrasound, cross-sectional imaging as indicated). These cutoffs can refine the shared decision-making discussion about scope of neck dissection and anticipated risk of nodal disease.
For researchers and guideline panels: these thresholds need prospective, ideally randomized, evaluation to determine whether biomarker-guided selective neck dissection improves oncologic outcomes (SRFS, disease-specific survival) and/or reduces morbidity compared with standard strategies. Harmonization of calcitonin assay reporting and local laboratory validation will be necessary before broad implementation.
Conclusion
This multicenter cohort study provides updated preoperative basal calcitonin thresholds, measured by modern immunoassays, that predict compartment-specific lymph node metastasis and better discriminate structural recurrence risk compared with older guideline cutoffs. These thresholds are a practical step toward precision surgical planning in MTC but require prospective validation and careful assay-specific application before becoming standard practice.
Funding and clinicaltrials.gov
Funding sources and trial registration details, if any, are reported in the original publication (Du et al., JAMA Otolaryngol Head Neck Surg. 2025). Readers should consult the primary manuscript for full disclosures and funding statements.
References
1. Du Y, Shen C, Song K, et al. Updated Thresholds of Basal Calcitonin Level and Extent of Lymph Node Metastasis in Initially Treated Medullary Thyroid Cancer. JAMA Otolaryngol Head Neck Surg. 2025 Aug 1;151(8):761-767. doi: 10.1001/jamaoto.2025.0542 IF: 5.6 Q1 . Erratum in: JAMA Otolaryngol Head Neck Surg. 2025 Nov 13. doi: 10.1001/jamaoto.2025.4384 IF: 5.6 Q1 . PMID: 40569620 IF: 5.6 Q1 ; PMCID: PMC12203393 IF: 5.6 Q1 .
2. Wells SA Jr, Asa SL, Dralle H, et al. Revised American Thyroid Association Guidelines for the Management of Medullary Thyroid Carcinoma. Thyroid. 2015;25(6):567–610. (American Thyroid Association MTC Guideline)
Suggested next steps for clinicians
– Review local calcitonin assay platform and reportable ranges; convert units where necessary and consider local cross-validation with the thresholds reported here before clinical adoption.
– Integrate calcitonin thresholds with high-resolution neck ultrasound and, when indicated, CT/MRI or PET imaging to guide decision-making about compartment-specific neck dissection.
– Engage patients in informed discussions about the trade-offs between more extensive initial surgery and potential morbidity versus the risk of recurrent disease that may require reoperation.
Authors’ note
This article synthesizes and interprets results from Du et al. (2025). Clinicians should consult the full original report and supplementary materials for methodological detail, and await prospective validation studies before changing standard practice.