Introduction: The Dilemma of Chronic Limb-Threatening Ischemia
Chronic limb-threatening ischemia (CLTI) represents the most advanced and morbid stage of peripheral artery disease (PAD). Characterized by rest pain, non-healing ulcers, or gangrene, CLTI carries a high risk of major amputation and cardiovascular mortality. For clinicians, the primary goal is revascularization to restore blood flow to the affected limb, yet the optimal method—surgical bypass or endovascular therapy—has been a subject of intense debate for decades.
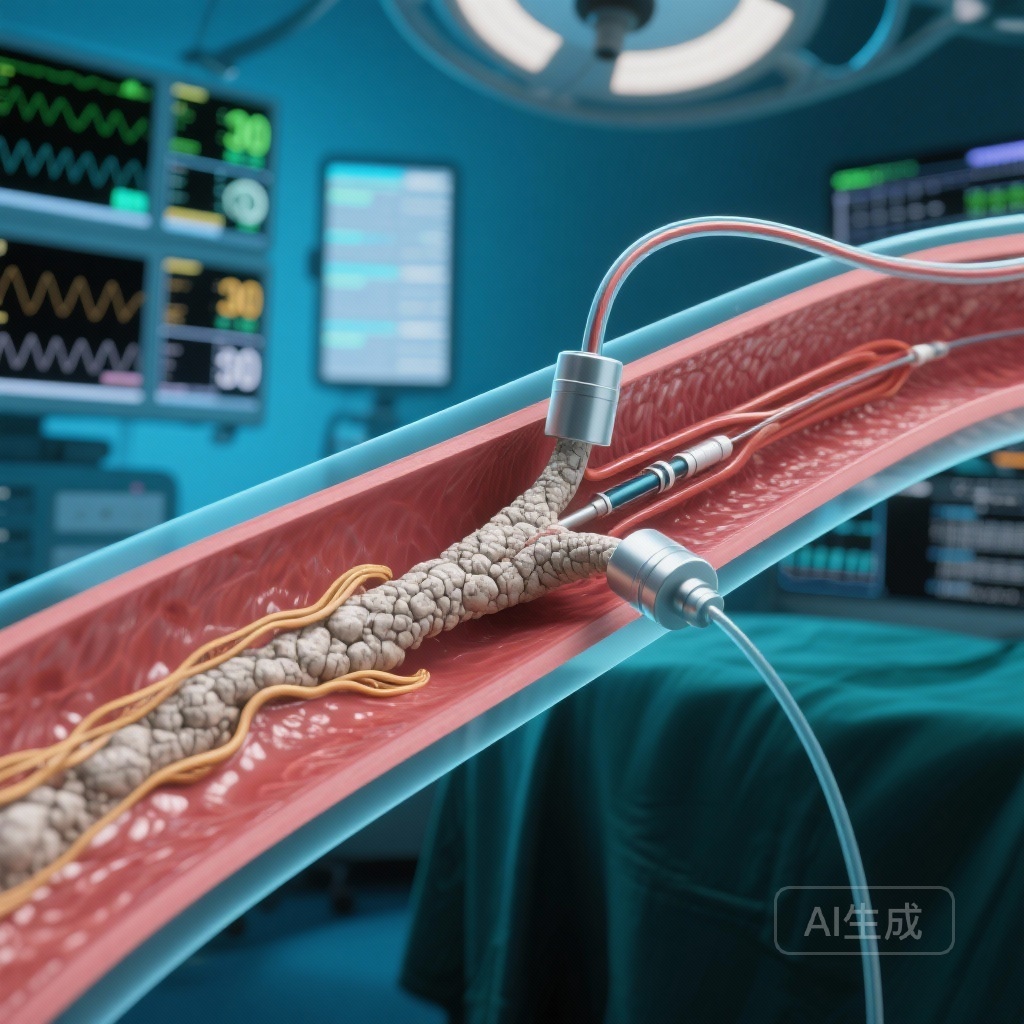
In recent years, endovascular techniques have seen a surge in technological advancements, including the widespread adoption of atherectomy. Atherectomy, the mechanical removal of plaque from the arterial wall, is theoretically appealing because it reduces the plaque burden and may decrease the need for high-pressure balloon angioplasty or stenting. However, while atherectomy has established roles in coronary interventions, its clinical efficacy in the peripheral vasculature—specifically for CLTI—has remained under-supported by high-quality, randomized evidence. A new analysis of the BEST-CLI trial, published in JACC: Cardiovascular Interventions, provides much-needed clarity on this controversial procedure.
The BEST-CLI Trial: A Robust Framework for Analysis
To understand the implications of atherectomy’s performance, one must first look at the foundation provided by the BEST-CLI (Best Endovascular vs. Best Surgical Therapy in Patients With CLTI) trial. This international, multicenter, randomized controlled trial was designed to compare the clinical effectiveness and safety of surgical bypass versus endovascular therapy in patients with CLTI and infrainguinal PAD.
The original trial, led by Farber et al. and published in the New England Journal of Medicine in 2022, divided patients into two cohorts. Cohort 1 consisted of patients with an adequate great saphenous vein (GSV) available for bypass, while Cohort 2 included patients who required an alternative conduit. The findings were landmark: in Cohort 1, surgical bypass with GSV was significantly superior to endovascular therapy in reducing major adverse limb events (MALE) and death. In Cohort 2, the outcomes between surgery and endovascular therapy were comparable.
Methodology: Evaluating Atherectomy within the Endovascular Cohort
Following the primary results, Hicks and colleagues performed a secondary analysis focusing specifically on the endovascular arm of the trial. Their objective was to determine whether the use of atherectomy during endovascular revascularization was associated with improved limb-based outcomes.
The study included 923 patients from the BEST-CLI trial who underwent an endovascular intervention. The researchers stratified this population into two groups: those treated with atherectomy (n=132, 14.3%) and those treated without atherectomy (n=791, 85.7%). The primary endpoint was MALE, defined as a composite of major reintervention (new bypass graft, graft revision, thrombectomy, or thrombolysis) or above-ankle amputation in the index limb.
Key Findings: Does Atherectomy Add Value?
Primary Outcomes and Hazard Ratios
The results of the analysis were striking. After adjusting for baseline risk factors, the researchers found that atherectomy was not associated with a reduction in MALE. The adjusted hazard ratio (aHR) for MALE was 1.30 (95% CI: 0.92-1.84), suggesting a trend toward worse outcomes, though it did not reach statistical significance in the overall adjusted model.
Similarly, individual components of the primary endpoint showed no benefit. Major reintervention rates (aHR: 1.07; 95% CI: 0.67-1.73), above-ankle amputation rates (aHR: 1.32; 95% CI: 0.81-2.15), and all-cause mortality (aHR: 1.06; 95% CI: 0.75-1.49) were all statistically similar between the atherectomy and non-atherectomy groups.
The Technical Success Paradox
Perhaps the most concerning finding emerged from a sensitivity analysis limited to patients in whom technical success was achieved during the index procedure. In this subgroup, the use of atherectomy was actually associated with a significantly higher risk of MALE (unadjusted log-rank P = 0.02; aHR: 1.51; 95% CI: 1.03-2.22). This suggests that even when the procedure is executed flawlessly from a technical standpoint, the biological or mechanical impact of atherectomy may be detrimental to long-term limb salvage compared to other endovascular modalities like balloon angioplasty or stenting alone.
Expert Commentary: Why the Lack of Benefit?
The failure of atherectomy to improve outcomes in this high-stakes population raises several clinical and mechanistic questions. Unlike the coronary arteries, the infrainguinal peripheral arteries are subject to significant mechanical stresses, including flexion, torsion, and compression. Atherectomy devices, while effective at debulking plaque, may cause significant barotrauma or deep vessel wall injury. This trauma can trigger an aggressive neointimal hyperglycemic response or facilitate distal embolization of plaque fragments into the microvasculature, which is already compromised in CLTI patients.
From a health policy perspective, these findings are particularly relevant. Atherectomy is a high-cost intervention, often reimbursed at significantly higher rates than balloon angioplasty, particularly in office-based labs (OBLs). The lack of clinical benefit, coupled with the potential for increased MALE, challenges the routine use of these devices without clearer evidence of superiority in specific lesion types, such as severely calcified vessels where standard balloons might fail.
Limitations and Future Directions
While this analysis is robust, it is a secondary analysis of a randomized trial, not a primary randomization to atherectomy itself. This introduces the possibility of selection bias, as the choice to use atherectomy was left to the discretion of the treating physician. Furthermore, the study did not differentiate between types of atherectomy (orbital, directional, laser, or rotational), which may have different safety profiles and efficacy levels.
Future research should focus on identifying specific anatomical or lesion-based characteristics that might actually benefit from atherectomy. Until then, the BEST-CLI data suggests that clinicians should exercise caution and prioritize evidence-based revascularization strategies—specifically surgical bypass with GSV when feasible—over high-cost, low-evidence endovascular add-ons.
Conclusion: Shaping the Future of Peripheral Revascularization
The analysis by Hicks et al. serves as a pivotal moment in vascular medicine. It reinforces the primary message of BEST-CLI: surgical revascularization remains the gold standard for many patients with CLTI. For those undergoing endovascular therapy, the addition of atherectomy does not appear to provide a safety net or an efficacy boost. Instead, it adds cost and may potentially worsen outcomes in certain scenarios. As the medical community moves toward value-based care, these results emphasize the need for rigorous, randomized data to justify the use of expensive medical technologies in the treatment of complex diseases like CLTI.
Funding and ClinicalTrials.gov Information
The BEST-CLI trial was funded by the National Heart, Lung, and Blood Institute (NHLBI). ClinicalTrials.gov number: NCT02060630.
References
1. Hicks CW, Farber A, Doros G, et al. Atherectomy Is Not Associated With Improved Limb-Based Outcomes Among Patients in the BEST-CLI Trial Undergoing Endovascular Revascularization. JACC Cardiovasc Interv. 2026;19(1):96-107.
2. Farber A, Menard MT, Conte MS, et al. Surgery or Endovascular Therapy for Chronic Limb-Threatening Ischemia. N Engl J Med. 2022;387(25):2305-2316.