Introduction: The Silent Threat to Neurocognitive Longevity
For decades, the impact of ambient air pollution on human health was primarily framed within the context of respiratory and cardiovascular diseases. However, a growing body of epidemiological evidence has shifted the focus toward the central nervous system, identifying fine particulate matter (PM2.5) and nitrogen oxides as significant modifiable risk factors for dementia. Despite the strong statistical associations between poor air quality and cognitive decline, the underlying biological pathways have remained somewhat elusive. Specifically, clinicians and researchers have questioned whether air pollution acts as a general systemic stressor or if it directly influences the characteristic neuropathological hallmarks of Alzheimer’s disease (AD).
Recent high-impact studies, including analyses of the University of Pennsylvania’s brain bank, the 1946 British Birth Cohort, and the UK Biobank, have provided groundbreaking insights. These studies demonstrate that the relationship between air pollution and dementia is not merely incidental but is mediated by specific neuropathological changes and systemic physiological pathways, such as pulmonary function. This article provides a critical interpretation of these findings, exploring how lifetime exposure to pollutants shapes the aging brain.
Evidence from Autopsy: PM2.5 and Alzheimer’s Neuropathologic Change
One of the most significant challenges in dementia research is confirming the relationship between environmental exposures and actual brain pathology, which can only be definitively assessed post-mortem. A landmark study published in JAMA Neurology (Kim et al., 2025) addressed this by examining 602 autopsy cases from the Center for Neurodegenerative Disease Research Brain Bank at the University of Pennsylvania.
The Penn Brain Bank Study: Methods and Cohort
The researchers analyzed cases collected between 1999 and 2022, focusing on individuals with various forms of dementia, movement disorders, and healthy controls. By utilizing spatiotemporal prediction models to estimate one-year mean PM2.5 concentrations at each participant’s residential address prior to death, the team was able to correlate pollution levels with ten specific neuropathologic measures, including those for Alzheimer’s disease (ADNC), Lewy body disease, and cerebrovascular disease.
Key Finding: Pathological Mediation of Cognitive Decline
The results were striking. Higher PM2.5 exposure was significantly associated with increased odds of more severe Alzheimer’s disease neuropathologic change (odds ratio, 1.19; 95% CI, 1.11-1.28). Furthermore, in a subset of cases where Clinical Dementia Rating Sum of Boxes (CDR-SB) scores were available, higher PM2.5 exposure correlated with greater cognitive and functional impairment (beta = 0.48).
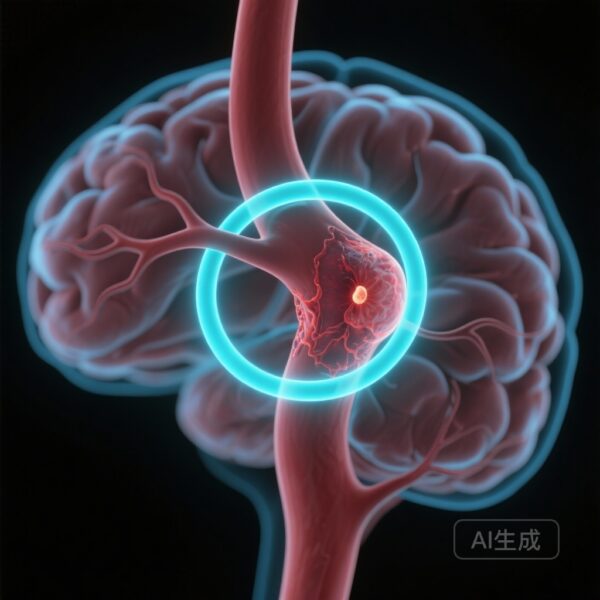
Crucially, structural equation modeling revealed that 63 percent of the association between PM2.5 exposure and cognitive impairment was statistically mediated by ADNC. This suggests that PM2.5 does not just exacerbate existing symptoms; it may actively drive the amyloid and tau pathology that defines Alzheimer’s disease. This finding provides a missing link in the neurotoxicological chain, suggesting that fine particles may either enter the brain directly via the olfactory bulb or trigger systemic inflammatory responses that accelerate neurodegenerative processes.
The Longitudinal Perspective: Insights from the 1946 British Birth Cohort
While the Penn study provided a cross-sectional look at end-of-life pathology, the Medical Research Council National Survey of Health and Development (the 1946 British Birth Cohort) offers a unique longitudinal perspective on how air pollution affects the brain over decades. As reported in Lancet Healthy Longevity (Canning et al., 2025), researchers followed participants from birth through their late 60s and early 70s.
Life Course Exposure and Midlife Cognitive Trajectories
The study assessed exposures to nitrogen dioxide (NO2) and particulate matter (PM10 and PM2.5) across midlife (ages 45 to 64). The findings indicated that higher exposure to NO2 and PM10 in midlife was associated with significantly slower processing speed between the ages of 43 and 69. For example, NO2 exposure showed a beta of -8.121 per interquartile range increase. Additionally, higher exposure to all tested pollutants was associated with lower scores on the Addenbrooke’s Cognitive Examination III (ACE-III) at age 69, a comprehensive measure of cognitive state.
Structural Neuroimaging: Ventricular and Hippocampal Changes
Perhaps the most compelling evidence from the British cohort came from neuroimaging. Using MRI data from the Insight 46 substudy, researchers found that higher exposure to nitrogen oxides (NOx) was associated with smaller hippocampal volume—a hallmark of early Alzheimer’s. Conversely, higher NO2 and PM10 exposures were associated with larger ventricular volumes, which often indicates overall brain atrophy. These structural changes provide objective evidence that air pollution contributes to accelerated brain aging and tissue loss, independent of other sociodemographic factors like smoking or neighborhood deprivation.
The Systemic Pathway: The Role of Pulmonary Function
If air pollution affects the brain, what are the physiological intermediaries? Research using the UK Biobank (Lin et al., 2024) explored the potential role of pulmonary function (PF) as a mediator. This study analyzed five major air pollutants and their cumulative mixture in relation to cognitive performance and dementia risk.
UK Biobank Analysis: Identifying Physiological Mediators
The study found that a mixture of air pollutants was negatively associated with performance across five cognitive tests and global cognition. Crucially, the researchers identified a significantly negative association between the air pollution mixture and pulmonary function. Mediation analysis revealed that pulmonary function accounted for approximately 6.08 percent of the association between air pollution and global cognition. Furthermore, pulmonary function was found to mediate the risk of dementia associated with NOx, NO2, and PM2.5.
This suggests a multi-hit hypothesis: air pollution compromises respiratory health, leading to chronic systemic hypoxia or the release of pro-inflammatory cytokines into the bloodstream, which then cross the blood-brain barrier to impair cognitive function. While the mediation percentage is modest, it highlights that the “lung-brain axis” is a critical component of environmental neurotoxicity.
Clinical Implications and Biological Plausibility
For clinicians, these studies underscore the importance of considering environmental history in the assessment of cognitive risk. The biological plausibility of these findings is supported by several mechanisms. First, ultra-fine particles can reach the brain directly via the olfactory nerve, bypassing the blood-brain barrier. Second, PM2.5 is known to induce oxidative stress and neuroinflammation, which are primary drivers of protein misfolding. Third, as shown in the UK Biobank study, the systemic inflammatory response triggered in the lungs can have secondary effects on cerebral vascular integrity and neuronal health.
Public Health and Policy Considerations
The evidence that 63 percent of the pollution-cognition link is mediated by ADNC (Kim et al.) and that midlife exposure predicts late-life brain atrophy (Canning et al.) suggests that the window for intervention is broad. Reducing ambient air pollution is not just a respiratory health initiative; it is a primary prevention strategy for dementia. Policy changes aimed at reducing NO2 from traffic and PM2.5 from industrial sources could significantly reduce the global burden of Alzheimer’s disease.
Conclusion: A Call for Environmental Neuroprotection
The convergence of pathological, longitudinal, and systemic data from these three major studies provides a compelling indictment of ambient air pollution as a neurotoxic threat. We now have evidence that pollution exposure is linked to the physical hallmarks of Alzheimer’s at autopsy, structural atrophy on MRI, and cognitive decline mediated by respiratory health.
Future research should focus on whether individual-level interventions, such as high-efficiency particulate air (HEPA) filtration or improved urban planning, can attenuate these risks. In the meantime, healthcare providers should recognize that the air their patients breathe is as much a determinant of brain health as their blood pressure or glucose levels. Protecting the brain requires protecting the environment.
References
1. Kim B, Blam K, Elser H, et al. Ambient Air Pollution and the Severity of Alzheimer Disease Neuropathology. JAMA Neurol. 2025;82(11):1153-1161. doi:10.1001/jamaneurol.2025.3316.
2. Canning T, Arias-de la Torre J, Fisher HL, et al. Associations between life course exposure to ambient air pollution with cognition and later-life brain structure: a population-based study of the 1946 British Birth Cohort. Lancet Healthy Longev. 2025;6(7):100724. doi:10.1016/j.lanhl.2025.100724.
3. Lin F, Wang L, Shi Y, et al. Association of Exposure to Ambient Air Pollutants With Cognitive Performance and Dementia Risk and the Mediating Role of Pulmonary Function: Evidence From the UK Biobank. J Gerontol A Biol Sci Med Sci. 2024;79(7):glae139. doi:10.1093/gerona/glae139.