Introduction: The Changing Face of AIFRS
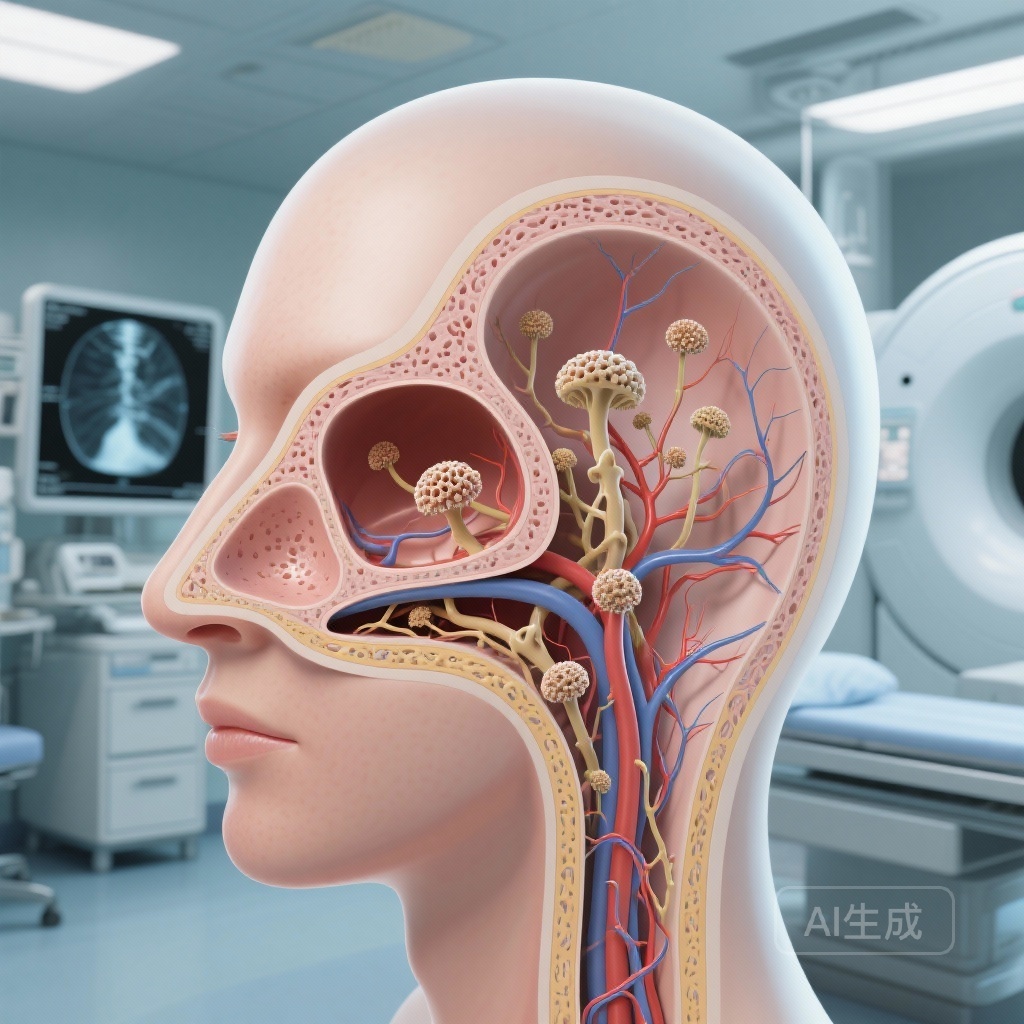
Acute invasive fungal rhinosinusitis (AIFRS) is a clinical emergency characterized by rapid fungal invasion of the sinonasal mucosa, often extending into the orbit and the cranial vault. Historically associated with dismal prognoses, this condition primarily strikes those with profound immune dysfunction, such as patients with hematologic malignancies, transplant recipients, and those with uncontrolled diabetes mellitus. As medical science advances in its ability to manage immunosuppression and provide targeted antifungal therapy, the clinical landscape of AIFRS has undergone a significant shift. A recent landmark systematic review and meta-analysis published in JAMA Otolaryngology–Head & Neck Surgery provides a critical update on the temporal trends in proportion, morbidity, and mortality of this lethal infection.
Disease Burden and Clinical Context
The pathophysiology of AIFRS is rooted in the opportunistic nature of fungi such as Aspergillus and the Mucorales order. In a healthy host, these spores are cleared by innate immune mechanisms. However, in the setting of neutropenia or ketoacidosis, these fungi germinate and exhibit angioinvasion, leading to tissue infarction and necrosis. This process can occur within hours, making early diagnosis the single most important factor for survival. Despite the integration of newer diagnostic tools like high-resolution CT and MRI, as well as the advent of potent triazoles and liposomal amphotericin B, the burden of the disease remains substantial for the growing population of immunocompromised individuals worldwide.
Study Design and Methodology
The study by Candelo et al. (2026) represents a monumental effort to synthesize data spanning over four decades. Following PRISMA guidelines, the researchers conducted an exhaustive search across Ovid MEDLINE, PubMed, Scopus, and other major databases from 1977 through October 2025. The inclusion criteria were rigorous, focusing on studies that reported proportion, morbidity, or mortality in immunocompromised cohorts with at least 10 patients.
A total of 205 studies were included, encompassing a staggering 48,437 immunocompromised patients. Of these, 10,311 were diagnosed with AIFRS. To understand the impact of modern medical advancements, the researchers stratified the data into two distinct periods: 1983-2012 and 2013-2025. Statistical analysis utilized random-effects meta-analysis and meta-regression to account for heterogeneity and temporal shifts.
Key Findings: Increased Detection and Improved Survival
A Rising Proportion of AIFRS
One of the most striking findings of the meta-analysis is the increase in the pooled proportion of AIFRS among immunocompromised patients. The overall proportion was 11.8%, but when looking at the modern era (2013-2025), this figure rose to 16.6%. This increase may not necessarily reflect a higher incidence of the infection itself, but rather a significant improvement in diagnostic sensitivity. Enhanced clinical awareness and the routine use of endoscopic surveillance in high-risk patients allow for the identification of cases that might have previously gone undiagnosed or were only identified post-mortem.
The Decline in Mortality
Perhaps the most encouraging data point is the substantial decline in mortality. The overall mortality rate was calculated at 31.2%. However, the temporal analysis revealed a drop from 41.9% in the pre-2013 era to 28.2% in the post-2013 era. This improvement is likely multifactorial, stemming from earlier surgical intervention, the availability of broader-spectrum antifungal agents like isavuconazole and voriconazole, and better management of the underlying immunosuppressive conditions (e.g., use of G-CSF to shorten neutropenic windows).
Stubborn Morbidity Rates
While survival has improved, morbidity remains high and relatively stable. The pooled morbidity rate was 37.0%, with no statistically significant difference between the two time periods (39.3% vs. 36.4%). The complications associated with AIFRS are often devastating, including permanent vision loss, exophthalmos, and the need for orbital exenteration. These findings underscore that while we are saving more lives, the aggressive nature of the disease still results in significant long-term disability for survivors.
Expert Commentary: Interpreting the Shift
The data presented in this meta-analysis offer a nuanced view of AIFRS in the 21st century. The rise in proportion alongside a fall in mortality suggests that we are entering an era of “proactive management.” In the past, AIFRS was often a terminal diagnosis found late in the disease course. Today, the integration of otorhinolaryngologists into the transplant and oncology teams ensures that patients with even minor sinonasal symptoms receive immediate endoscopic evaluation.
However, the high morbidity rates highlight a persistent challenge: the balance between aggressive surgical debridement and functional preservation. Orbital involvement remains a critical decision point for surgeons. The frequency of vision loss and exenteration mentioned in the study confirms that once the fungus traverses the lamina papyracea, the therapeutic window narrows rapidly. Future research should focus on refining the timing of surgery and the potential role of local antifungal irrigation as an adjunct to systemic therapy.
Conclusion: Clinical Implications and Future Directions
This systematic review confirms that the clinical outlook for patients with AIFRS is improving, yet the disease remains a formidable opponent. The reduction in mortality to below 30% is a testament to the progress in multidisciplinary care. Nonetheless, the stability of morbidity rates serves as a sobering reminder of the destructive power of invasive fungi.
For clinicians, the message is clear: maintaining a high index of suspicion in immunocompromised populations is vital. Early diagnostic endoscopy and biopsy remain the gold standard. As the population of patients undergoing advanced immunotherapy and organ transplantation grows, the medical community must continue to refine these strategies to further reduce both the mortality and the life-altering morbidity associated with this infection.
References
1. Candelo E, Vasudevan SS, Osuoha GC, et al. Proportion, Morbidity, and Mortality of Acute Invasive Fungal Rhinosinusitis in Immunocompromised Populations: A Systematic Review and Meta-analysis. JAMA Otolaryngol Head Neck Surg. 2026;e255077. doi:10.1001/jamaoto.2025.5077.
2. Turner JH, Goldberg AN. The role of endoscopic sinus surgery in the management of acute invasive fungal rhinosinusitis. Am J Rhinol Allergy. 2021;35(4):450-458.
3. Spellberg B, Edwards J Jr, Ibrahim A. Novel perspectives on mucormycosis: pathophysiology, diagnosis, and treatment. Clin Microbiol Rev. 2005;18(3):556-569.