Highlights
- A deep learning-based muscle-bone ratio (MBR) serves as a potent predictive biomarker for anti-EGFR therapy efficacy in RAS wild-type metastatic colorectal cancer (mCRC).
- In the PanaMa trial, patients with a high MBR receiving panitumumab maintenance showed significantly longer progression-free survival (HR 0.43) and overall survival (HR 0.41).
- Conversely, patients with low MBR derived no significant benefit from the addition of panitumumab to FU/FA maintenance therapy.
- These findings were validated in an independent real-world cohort, highlighting the potential for automated CT-based body composition analysis in clinical decision-making.
Introduction: The Unmet Need in mCRC Maintenance Therapy
The management of metastatic colorectal cancer (mCRC) has been revolutionized by the identification of molecular biomarkers, most notably the RAS and BRAF mutational status. For patients with RAS wild-type (WT) tumors, anti-epidermal growth factor receptor (anti-EGFR) therapies like panitumumab and cetuximab are standard-of-care components. However, even within molecularly defined subgroups, clinical response remains heterogeneous. Current clinical trials often fail to account for host-related factors—such as nutritional status and body composition—that significantly influence drug metabolism, toxicity, and overall survival.
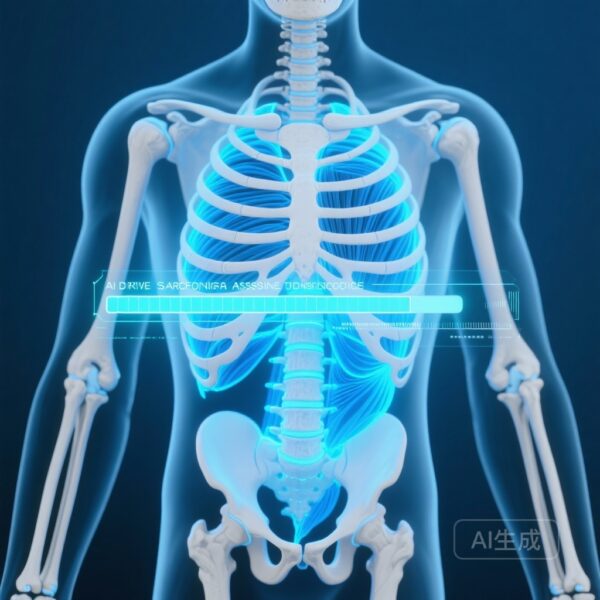
Sarcopenia, the progressive loss of skeletal muscle mass and strength, is increasingly recognized as a critical prognostic factor in oncology. Traditionally, assessing sarcopenia required manual, time-consuming segmentation of computed tomography (CT) images by specialized radiologists. The advent of deep learning (DL) has now enabled automated, high-throughput body composition analysis, allowing for the extraction of skeletal muscle and bone metrics from routine clinical imaging. This study investigates whether an AI-derived muscle-bone ratio (MBR) can predict which patients truly benefit from treatment intensification with anti-EGFR agents.
Study Design: The PanaMa Trial and AI Integration
The researchers utilized data from the prospective PanaMa study (AIO KRK 0212; NCT01991873), a randomized phase II trial. The trial enrolled patients with RAS WT mCRC who had achieved at least stable disease following induction therapy with 5-fluorouracil, folinic acid, oxaliplatin (mFOLFOX6), and panitumumab. Patients were randomized to receive maintenance therapy with either fluorouracil and folinic acid (FU/FA) alone or FU/FA plus panitumumab (Pmab).
To assess the host-related factor of sarcopenia, the investigators applied a validated deep learning model to pre-maintenance CT images. This model automatically segmented skeletal muscle and bone areas at the level of the third lumbar vertebra (L3). The primary metric derived was the Muscle-Bone Ratio (MBR), which accounts for skeletal frame size. Patients were stratified into tertiles based on their MBR. The primary endpoints for this post-hoc analysis were progression-free survival (PFS) and overall survival (OS), analyzed via Kaplan-Meier estimates and Cox proportional hazards regression. To ensure the robustness of the findings, a retrospective real-world validation cohort of mCRC patients treated with cetuximab was also analyzed.
Key Findings: MBR as a Predictive and Prognostic Biomarker
Of the 248 patients randomized in the PanaMa trial, pre-maintenance CT images were available for 189 (76.2%). The analysis revealed a striking divergence in treatment outcomes based on the AI-derived sarcopenia marker.
Predictive Value of MBR
The most significant finding was that the benefit of panitumumab was heavily dependent on the patient’s MBR. In the high-MBR tertile, the addition of panitumumab to FU/FA led to a substantial reduction in the risk of progression (HR 0.42, 95% CI: 0.24-0.73, P=0.002). In contrast, for patients in the lower MBR groups, there was no statistically significant difference in PFS between the FU/FA+Pmab and FU/FA-only arms. This suggests that the MBR is not merely a prognostic indicator of health but a predictive biomarker for anti-EGFR efficacy.
Survival Outcomes in the PanaMa Cohort
Within the group receiving FU/FA+Pmab, patients with a high MBR experienced significantly superior outcomes compared to those with lower MBRs. Specifically:
- Progression-Free Survival (PFS): HR 0.43 (95% CI: 0.25-0.73, P=0.002).
- Overall Survival (OS): HR 0.41 (95% CI: 0.21-0.77, P=0.006).
Interestingly, in the cohort receiving FU/FA alone, the MBR did not correlate with survival outcomes, reinforcing the idea that MBR specifically modulates the response to anti-EGFR therapy rather than just reflecting a general fitness for any chemotherapy.
Validation in the Real-World Cohort
The predictive power of the MBR was further confirmed in an independent real-world cohort of patients treated with cetuximab. In this group, high MBR was again associated with superior PFS (P=0.002) and OS (P<0.001). The consistency of results across both a controlled clinical trial and a real-world setting underscores the reliability of automated sarcopenia assessment as a clinical tool.
Expert Commentary: Mechanistic Insights and Clinical Implications
The biological plausibility of these findings is rooted in the complex interplay between host metabolism and tumor biology. Sarcopenia is often a manifestation of cancer cachexia, a systemic inflammatory state characterized by elevated pro-inflammatory cytokines such as IL-6 and TNF-alpha. These cytokines can activate alternative signaling pathways (e.g., STAT3 or MAPK) that bypass EGFR inhibition, potentially leading to primary or acquired resistance to panitumumab and cetuximab.
Furthermore, skeletal muscle acts as a metabolic sink and an endocrine organ. Sarcopenic patients often exhibit altered pharmacokinetics, leading to higher relative drug concentrations and increased toxicity, which may necessitate dose reductions or treatment interruptions, thereby limiting efficacy. By using the MBR—which normalizes muscle mass to bone area—clinicians can obtain a more accurate reflection of a patient’s physiological reserve than Body Mass Index (BMI) or body surface area (BSA) alone.
From a clinical perspective, this study suggests that for patients with low MBR, the toxicity and cost of panitumumab intensification during maintenance may not be justified by the marginal clinical benefit. Conversely, for patients with high MBR, panitumumab remains a highly effective strategy that significantly extends survival.
Study Limitations and Future Directions
While the study provides compelling evidence, several limitations must be considered. First, this was a post-hoc analysis of the PanaMa trial; prospective validation in a trial specifically stratified by MBR is required to confirm these findings as level 1 evidence. Second, while the AI model is validated, the specific thresholds for MBR tertiles may vary across different populations and CT scanners, necessitating standardization before widespread clinical adoption.
Future research should investigate whether nutritional interventions or exercise programs designed to reverse sarcopenia can convert “non-responders” (low MBR) into “responders” (high MBR) for anti-EGFR therapy. Additionally, integrating MBR with other biomarkers, such as circulating tumor DNA (ctDNA) or radiomics, could lead to even more refined personalized treatment algorithms.
Conclusion
The study by Keyl et al. demonstrates that automated, deep learning-derived sarcopenia markers provide critical insights into the efficacy of anti-EGFR therapy in mCRC. By showing that the benefit of panitumumab is largely confined to patients with a high muscle-bone ratio, the researchers have identified a practical, image-based tool for personalizing cancer care. As AI-driven body composition analysis becomes more integrated into diagnostic workflows, it promises to bridge the gap between molecular profiling and host-related physiology, ensuring that treatment intensification is reserved for those most likely to benefit.
Funding and clinicaltrials.gov
The PanaMa trial (AIO KRK 0212) was supported by Amgen and various academic grants. ClinicalTrials.gov Identifier: NCT01991873.
References
- Keyl J, Hosch R, Hörst F, et al. Deep Learning-derived Sarcopenia Marker Predicts Benefit from Anti-EGFR Therapy in Patients with RAS Wild-Type Metastatic Colorectal Cancer. Clin Cancer Res. 2026. doi: 10.1158/1078-0432.CCR-25-3080.
- Modest DP, Kartheuser R, Magg G, et al. Panitumumab Plus Fluorouracil and Folinic Acid Versus Fluorouracil and Folinic Acid Alone as Maintenance Therapy in RAS Wild-Type Metastatic Colorectal Cancer: The PanaMa Trial (AIO KRK 0212). J Clin Oncol. 2022;40(1):72-82.
- Fearon K, Strasser F, Anker SD, et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 2011;12(5):489-495.