Highlights
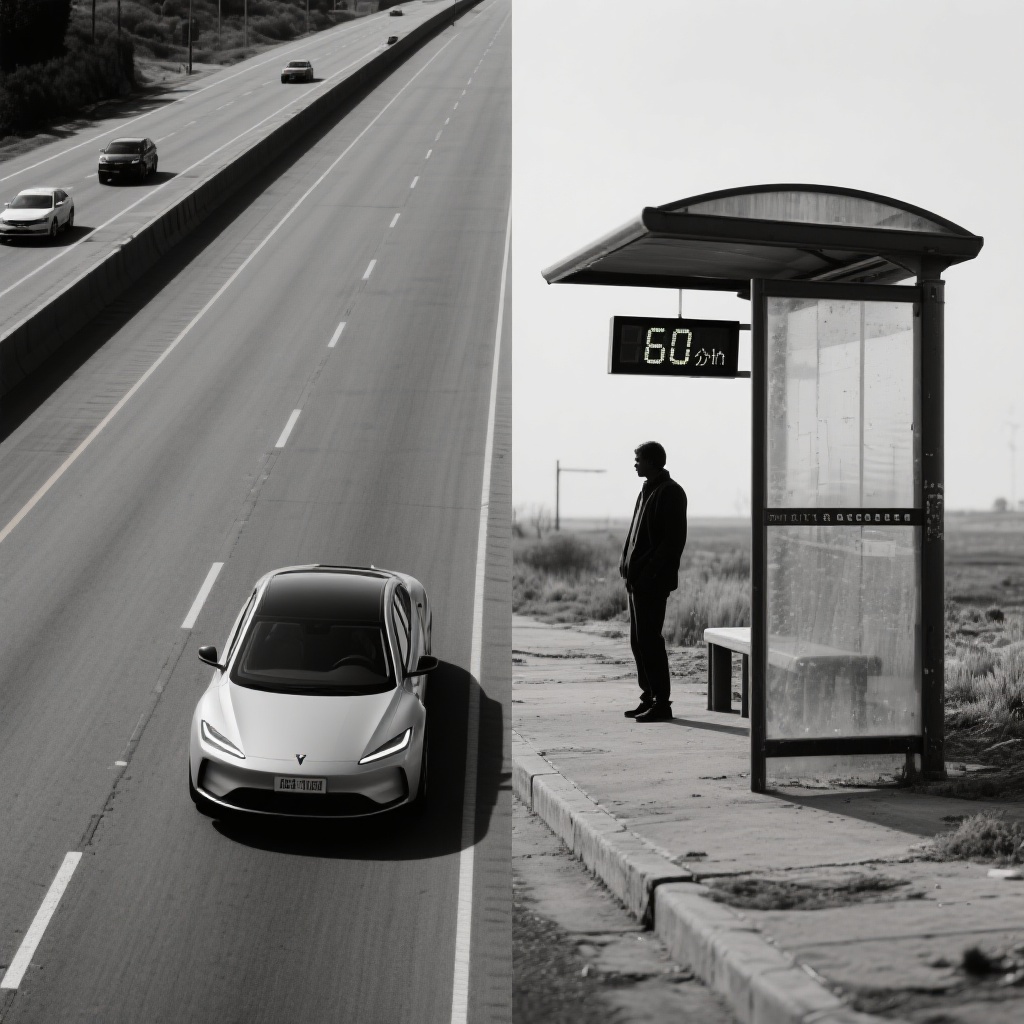
Public transit travel times to methadone clinics are approximately 300% to 400% longer than personal vehicle travel times, creating a significant ‘time tax’ for the most vulnerable patients.
More than half of the census block groups in Connecticut lack adequate public transit access to the nearest Opioid Treatment Program (OTP), defined as travel times exceeding 60 minutes or no available route.
Even in areas with the highest overdose death rates, transit-dependent individuals face nearly 40-minute commutes each way for a medication that often requires daily attendance.
Current federal regulations are identified as the primary structural barrier, necessitating a shift toward decentralized care, mobile services, and expanded take-home dose protocols.
The Methadone Access Crisis: A Structural Bottleneck
Methadone remains one of the most effective treatments for opioid use disorder (OUD), proven to reduce illicit opioid use, decrease overdose mortality, and improve social functioning. However, unlike buprenorphine, which can be prescribed in office-based settings and picked up at retail pharmacies, methadone for OUD is strictly regulated under federal law (42 CFR Part 8). It must be dispensed through highly specialized Opioid Treatment Programs (OTPs), which often require patients to attend in person for daily observed dosing, especially during the early stages of recovery.
This requirement for daily attendance transforms geographic distance into a daily logistical hurdle. For patients without reliable personal transportation, the ‘spatial mismatch’ between where they live and where clinics are located becomes a determinant of treatment retention. While previous research has mapped travel distances, few studies have critically compared the lived experience of travel via personal vehicle versus the often-unreliable infrastructure of public transit.
Study Design and Geospatial Methodology
In a comprehensive cross-sectional study published in JAMA Network Open, researchers led by Howell et al. conducted a geospatial analysis of the state of Connecticut in 2023. The study aimed to estimate and compare the median travel times to the nearest OTP via personal vehicle versus public transit across all 2,702 census block groups (CBGs) in the state.
The researchers utilized k-nearest neighbor spatial weight matrices and spatial error models to assess the associations between sociodemographic characteristics—including race, ethnicity, household income, and car ownership—and travel times. The analysis also integrated per-capita opioid overdose death rates to determine if treatment availability aligned with the areas of highest clinical need. Public transit data included bus and rail schedules, walking distances to stops, and transfer times, providing a realistic estimate of the burden faced by transit-dependent populations.
Key Findings: The Four-Fold Transit Penalty
The results of the analysis reveal a stark disparity in accessibility. Across all CBGs in Connecticut, the median travel time to the closest OTP was 11.0 minutes by personal vehicle. In contrast, the median travel time via public transit was 41.7 minutes. This represents nearly a four-fold increase in the time required to access life-saving medication.
The Transit Desert
The study found that 1,431 CBGs (53% of the state) were essentially ‘transit deserts’ regarding methadone access. These areas either had no available public transit trip to an OTP or required a travel time exceeding 60 minutes one way. When considering a daily dosing requirement, a 60-minute one-way trip equates to at least two hours of travel per day, not including time spent within the clinic. For a patient attempting to maintain employment or childcare, this ‘time tax’ is often prohibitive.
Disparities in High-Need Areas
One of the most concerning findings involved areas with the highest per-capita overdose death rates. In the 489 CBGs identified as overdose hotspots, the median travel time was 8.2 minutes by car but 37.6 minutes by public transit. Furthermore, 34% of these high-overdose areas lacked adequate public transit access entirely. This suggests that even when clinics are located near high-need urban centers, the lack of granular transit infrastructure leaves a significant portion of the population underserved.
Urban-Rural Gradients and Demographics
The study also identified that travel times via public transit increased significantly along the urban-rural gradient. While urban centers generally had better transit connectivity, suburban and rural areas saw travel times skyrocket. Additionally, travel times were longer in CBGs with a higher percentage of non-Hispanic White residents, reflecting the historical concentration of OTPs in urban, often racially diverse, lower-income neighborhoods—a legacy of ‘not-in-my-backyard’ (NIMBY) policies that have restricted clinic placement in suburban areas.
Clinical and Policy Implications
The findings by Howell et al. underscore that the barrier to methadone is not merely geographic distance, but the intersection of transit poverty and restrictive federal policy. If a patient is required to visit a clinic six days a week and spends 80 minutes in transit daily, they are spending over 30 hours a month just to receive their medication. This is a burden not seen in almost any other area of chronic disease management.
The Need for Decentralization
The authors argue that the current OTP model is outdated and fails to meet the needs of a modern patient population. Potential interventions include:
1. Mobile Treatment Units: Expanding the use of mobile vans that can bring methadone to transit-starved areas or overdose hotspots.
2. Pharmacy-Based Dispensing: Transitioning toward a model where stable patients can pick up methadone at retail pharmacies, similar to the systems used in the United Kingdom, Canada, and Australia.
3. Expanded Take-Home Doses: Leveraging the flexibilities introduced during the COVID-19 pandemic to allow more patients to receive multi-day supplies of medication, thereby reducing the frequency of required travel.
Expert Commentary and Limitations
Clinicians in the field of addiction medicine have long noted that ‘transportation issues’ are the most cited reason for missed doses and treatment dropout. This study provides the empirical data necessary to advocate for systemic change. However, some limitations must be considered. The study was conducted in Connecticut, a relatively small and densely populated state with a centralized transit system; travel disparities in larger, more rural states in the Midwest or South are likely even more extreme.
Furthermore, the study assumes that patients will always go to the ‘nearest’ OTP. In reality, patients may be forced to travel to a more distant clinic due to insurance coverage, waitlists, or specific service needs, meaning these findings likely represent a ‘best-case scenario’ for travel times.
Conclusion
The study by Howell et al. serves as a critical indictment of the current regulatory framework for methadone. While the medication itself is highly effective, the ‘clinic-only’ dispensing model creates a massive logistical barrier for those without cars. Reducing the travel-based barriers to methadone is not just a matter of improving bus routes; it requires a fundamental shift in federal policy to allow for more flexible, patient-centered care. Until the ‘time tax’ on recovery is eliminated, the full potential of methadone to curb the overdose epidemic will remain out of reach for many.
References
Howell BA, Kim J, Thornhill TA, Lee J, Biegacki ET, Grau LE, Fiellin DA, Heimer R, Gonsalves GS. Travel Time to Methadone Treatment Via Personal Vehicle vs Public Transit. JAMA Netw Open. 2026 Feb 2;9(2):e2557361. doi: 10.1001/jamanetworkopen.2025.57361. PMID: 41632474; PMCID: PMC12869344.