Highlights
- Potent P2Y12 inhibitor monotherapy (prasugrel or ticagrelor) initiated within 4 days of PCI for ACS significantly increases the risk of ischemic events within the first 30 days compared to standard DAPT.
- The early ischemic risk was nearly double in the monotherapy group (3.3% vs. 1.8%) during the first month.
- Aspirin withdrawal was consistently associated with lower bleeding rates both in the acute phase (0-30 days) and the maintenance phase (31-365 days).
- Between 31 and 365 days, ischemic outcomes were identical between groups, suggesting that the ‘ischemic penalty’ of monotherapy is confined to the early post-procedural period.
Introduction: The Shifting Paradigm of Antiplatelet Therapy
For decades, dual antiplatelet therapy (DAPT) combining aspirin with a P2Y12 inhibitor has been the cornerstone of management following percutaneous coronary intervention (PCI), particularly in the high-risk setting of acute coronary syndrome (ACS). However, the major drawback of DAPT is the increased risk of bleeding, which is independently associated with higher mortality. This has led to a growing interest in ‘aspirin-free’ strategies, where P2Y12 inhibitor monotherapy is used to mitigate bleeding while maintaining antithrombotic protection.
Recent trials such as TWILIGHT and TICO have shown that dropping aspirin after a short period of DAPT (usually 3 months) can reduce bleeding without increasing ischemic events. However, the NEOMINDSET trial took a bolder step by testing the withdrawal of aspirin almost immediately after PCI. This landmark analysis of the NEOMINDSET trial provides essential insights into the temporal distribution of these risks, answering a critical clinical question: how early is too early to stop aspirin?
Study Design and Methodology
The NEOMINDSET trial was a randomized, multicenter study that enrolled 3,410 patients with ACS who underwent successful PCI with drug-eluting stents (DES). Patients were randomized within 4 days of hospital admission to one of two strategies for a 12-month duration:
1. Monotherapy Group
Potent P2Y12 inhibitor monotherapy (either prasugrel 10 mg daily or ticagrelor 90 mg twice daily).
2. DAPT Group
Standard dual antiplatelet therapy consisting of aspirin (100 mg daily) plus a potent P2Y12 inhibitor.
This prespecified landmark analysis divided the follow-up into two distinct periods: the acute phase (0 to 30 days) and the maintenance phase (31 to 365 days). The co-primary ischemic outcome was a composite of all-cause death, myocardial infarction (MI), stroke, or urgent target-vessel revascularization (TVR). The co-primary bleeding outcome was defined as Bleeding Academic Research Consortium (BARC) type 2, 3, or 5 bleeding.
Key Findings: The Ischemic-Bleeding Trade-off
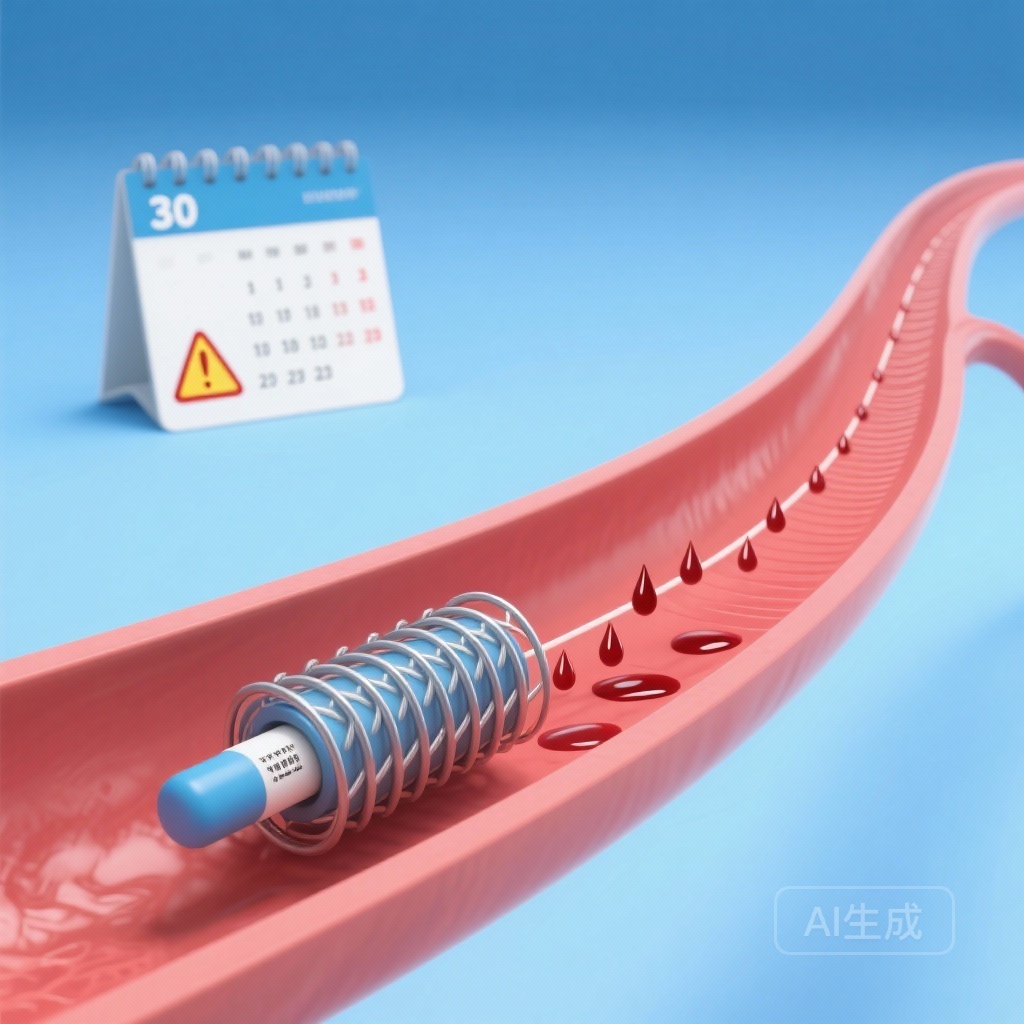
The Acute Phase (0-30 Days): A High-Risk Window
The first 30 days following PCI are characterized by a pro-thrombotic environment due to the recent plaque rupture and the procedural trauma to the vessel wall. In this landmark analysis, the monotherapy strategy failed to provide sufficient protection during this vulnerable window. The composite ischemic outcome occurred in 3.3% of the monotherapy group compared to only 1.8% in the DAPT group. This represents a statistically significant absolute risk difference of 1.5% (95% CI 0.4%-2.6%; P = .006).
Conversely, the reduction in bleeding was evident even in this early stage. Bleeding events occurred in 0.6% of patients on monotherapy versus 1.5% on DAPT (risk difference -0.8%; P = .018). While the reduction in bleeding is beneficial, the nearly twofold increase in ischemic events suggests that aspirin provides a critical safety net during the initial month of stent endothelialization.
The Maintenance Phase (31-365 Days): Safety Without Penalty
The results shifted dramatically after the first month. From day 31 to day 365, the ischemic outcome rates were identical between the two groups, both sitting at 3.8% (P = .977). This suggests that once the initial high-risk period has passed, monotherapy with a potent P2Y12 inhibitor is sufficient to prevent major adverse cardiovascular events.
Importantly, the bleeding benefit of monotherapy became even more pronounced during this late phase. Bleeding occurred in 1.3% of the monotherapy group compared to 3.5% in the DAPT group (risk difference -2.2%; P < .001). This confirms that the long-term continuation of aspirin contributes significantly to bleeding burden without providing additional ischemic protection after the first 30 days.
Clinical Interpretation and Expert Commentary
The findings from the NEOMINDSET landmark analysis have profound implications for clinical practice. They suggest that the ‘sweet spot’ for aspirin withdrawal in ACS patients is likely not within the first few days of PCI. The 83% relative increase in ischemic risk during the first 30 days with monotherapy is a signal that cannot be ignored.
Mechanistically, the early post-PCI period involves intense platelet activation and inflammatory responses. Aspirin, via its irreversible inhibition of cyclooxygenase-1 (COX-1), provides a different pathway of platelet inhibition than P2Y12 inhibitors. In the acute setting, this dual-pathway blockade seems necessary to prevent stent-related and non-stent-related ischemic events. Once the inflammatory milieu stabilizes and stent struts begin to endothelialize, the incremental benefit of aspirin diminishes, leaving only its bleeding risk.
It is also worth noting that NEOMINDSET utilized potent P2Y12 inhibitors (prasugrel and ticagrelor). Even with these high-potency agents, which provide more consistent and stronger platelet inhibition than clopidogrel, the absence of aspirin led to an early ischemic deficit. This differs from trials like TWILIGHT, where patients received 3 months of DAPT before switching to monotherapy, showing no ischemic increase. The NEOMINDSET data effectively bridges the gap, suggesting that while monotherapy is a viable long-term strategy, the transition should likely occur after at least 30 days of DAPT.
Conclusion and Future Directions
The NEOMINDSET landmark analysis reinforces the necessity of a nuanced approach to antiplatelet therapy. While the medical community is moving toward shorter DAPT durations to minimize bleeding, ‘ultra-short’ DAPT (less than 30 days) in ACS patients appears to carry a significant ischemic cost. Clinicians should maintain DAPT for at least the first month post-PCI in ACS patients to navigate the early ischemic danger zone, after which aspirin can be safely discontinued to reap the long-term benefits of reduced bleeding.
Future research should focus on whether specific high-bleeding-risk subgroups might still benefit from very early aspirin withdrawal, or if newer antithrombotic agents can bridge the gap without the ischemic penalty observed here.
References
1. Tavares CAM, et al. Prasugrel or ticagrelor monotherapy vs dual antiplatelet treatment after percutaneous coronary intervention in acute coronary syndromes: a landmark analysis from the NEOMINDSET trial. Eur Heart J. 2025. doi: 10.1093/eurheartj/ehaf1050.
2. Mehran R, et al. Ticagrelor with or without Aspirin in High-Risk Patients after PCI (TWILIGHT). N Engl J Med. 2019;381(21):2031-2042.
3. Kim BK, et al. Effect of Ticagrelor Monotherapy vs Ticagrelor with Aspirin on Major Bleeding and Cardiovascular Events in Patients With Acute Coronary Syndrome: The TICO Randomized Clinical Trial. JAMA. 2020;323(23):2407-2416.