Highlight
• A pooled analysis of 17 studies (2019–2024) found that individuals with type 2 diabetes have 4.19 times the odds of hearing loss compared with controls (95% CI 1.22–14.37).
• Diabetic participants had higher mean pure-tone thresholds overall (mean difference 3.19 dB), with a larger effect at high frequencies (2.3 dB) than low frequencies (1.11 dB).
• Longer diabetes duration (>10 years) and higher HbA1c were significantly associated with greater prevalence and severity of hearing impairment.
Background
Hearing loss is a common, often under-recognized chronic condition that reduces communication, social participation, and quality of life. In parallel, type 2 diabetes mellitus (T2DM) is a major global public health problem with multisystem complications affecting the vasculature and peripheral nerves. Observational data over decades have suggested an association between diabetes and auditory dysfunction, but estimates of magnitude and relevance to clinical care have varied. The recent PRISMA systematic review and meta-analysis by Caballero-Borrego and Andujar-Lara (2025) synthesizes contemporary evidence (articles published 2019–April 2024) to quantify the association between T2DM and hearing loss and to explore modifiers such as disease duration and glycaemic control.
Study design
Caballero-Borrego and Andujar-Lara searched PubMed and Scopus for relevant studies published between January 2019 and April 2024. Inclusion criteria centered on studies reporting prevalence or measures of hearing loss in adults with type 2 diabetes versus non-diabetic controls. Quality assessment and risk-of-bias evaluation used the Newcastle–Ottawa Scale. The authors pooled binary outcomes and continuous audiometric thresholds using Cochrane Review Manager (RevMan), and they examined subgroups including frequency-specific thresholds, diabetes duration, HbA1c, and sex.
Key findings
Study selection and overall prevalence
From 8,354 articles initially identified, 17 met inclusion criteria. Reported prevalence of hearing loss among persons with T2DM across included studies ranged widely from 40.6% to 71.9% — reflecting differences in populations, hearing-loss definitions, and assessment methods.
Odds of hearing loss in type 2 diabetes
When compared with control groups, persons with T2DM had markedly increased odds of hearing loss: pooled odds ratio (OR) 4.19 (95% confidence interval [CI] 1.22–14.37). The wide CI signals heterogeneity between studies and/or limited numbers in some pooled analyses, but the point estimate indicates a clinically meaningful association.
Audiometric thresholds — magnitude and frequency pattern
Continuous audiometric data showed that mean pure-tone thresholds in the diabetic group were 3.19 dB higher overall (95% CI 1.08–5.19). When stratified by frequency bands, low-frequency thresholds were 1.11 dB higher (95% CI 0.62–1.57), while high-frequency thresholds were disproportionately affected with a mean increase of 2.3 dB (95% CI 1.97–2.63). These findings point to a preferential impact on high-frequency hearing (typical early pattern in metabolic or noise-related cochlear injury), which is clinically important because high-frequency loss impairs speech discrimination, especially in noisy environments.
Glycemic control and hearing severity
Higher HbA1c levels correlated with greater hearing impairment. Patients classified with moderate hearing loss had mean HbA1c higher by 0.57% (95% CI 0.10–1.05) compared with controls; those with severe-to-profound loss had mean HbA1c higher by 0.95% (95% CI 0.02–1.87). While absolute differences appear modest, these are meaningful at the population level and suggest a dose–response relationship between hyperglycemia and auditory dysfunction.
Duration of diabetes and sex differences
Duration of diabetes emerged as a clear modifier: a diagnosis longer than 10 years was associated with higher odds of hearing loss (OR 2.07, 95% CI 1.45–2.94). In contrast, pooled analyses did not find a significant influence of sex on the association between T2DM and hearing loss.
Quality, heterogeneity, and limitations in pooled estimates
Quality assessment using the Newcastle–Ottawa Scale showed variable study quality. Heterogeneity across pooled estimates likely reflects differences in study design (cross-sectional vs. cohort), hearing-loss definitions (self-report vs. audiometry; threshold cutoffs), age distributions, noise exposure histories, ototoxic medication use, and adjustment for comorbidities such as cardiovascular disease. The substantial heterogeneity evident in some meta-analyses limits the precision with which we can estimate a single pooled effect size but does not negate the consistent direction of association across studies.
Expert commentary and biological plausibility
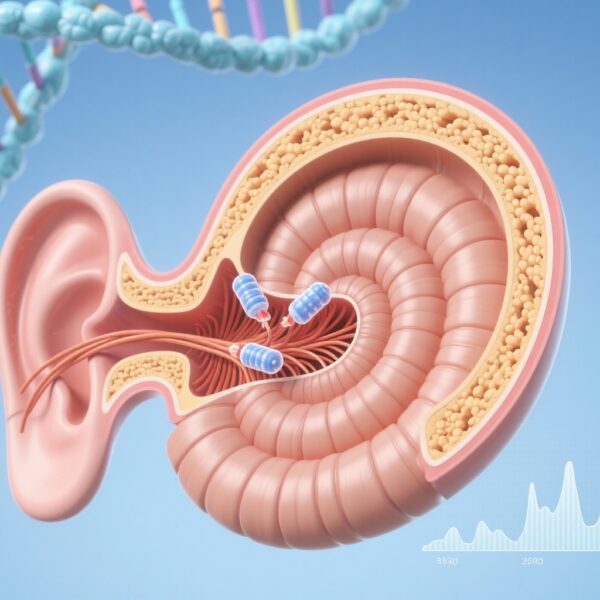
Multiple biologic mechanisms plausibly link T2DM to cochlear dysfunction. Chronic hyperglycemia is associated with microvascular disease and basement membrane thickening, which can reduce blood flow to the cochlea and stria vascularis leading to sensorineural damage. Diabetic neuropathy may affect the auditory nerve, and metabolic stress—oxidative injury and accumulation of advanced glycation end-products—may impair hair cell function. These pathophysiologic pathways align with the observed predilection for high-frequency loss, which arises from basal cochlear vulnerability.
From a clinical standpoint, the meta-analysis reinforces the view that hearing assessment should be considered in comprehensive diabetes care — especially for adults with long-standing disease or suboptimally controlled hyperglycemia. Early detection could facilitate timely audiologic rehabilitation (hearing aids, counseling) and potentially enable tighter metabolic control or targeted interventions to slow progression.
Implications for clinicians and policy
Practical takeaways for clinicians caring for adults with T2DM include the following:
- Maintain a low threshold for screening for hearing complaints; ask routinely about hearing difficulty and communication challenges, particularly in patients with >10 years diabetes duration or elevated HbA1c.
- Consider baseline audiometry (including high-frequency testing when available) for patients with long-standing disease or unexplained communication problems; repeat testing if symptoms progress.
- Address modifiable contributors to hearing loss — optimize glycemic control, review and minimize ototoxic medications where possible, counsel on noise exposure and smoking cessation, and manage cardiovascular risk factors.
- Refer to audiology and ENT for evaluation and management (hearing aids, assistive listening devices, tinnitus management) when indicated; integrate communication strategies into diabetes self-management education.
Study limitations, research gaps, and future directions
Key limitations of the available evidence include predominance of cross-sectional designs that preclude firm causal inference, heterogeneous outcome definitions, variable accounting for key confounders (e.g., cumulative noise exposure, ototoxic drug exposure, socioeconomic status), and relatively small study numbers for some subgroup analyses. The wide CI around the pooled OR indicates imprecision and between-study variability.
Priority research questions include prospective cohort studies with standardized, frequency-specific audiometry and robust adjustment for confounders; randomized trials testing whether improved glycemic control or other metabolic interventions reduce incidence or progression of hearing loss; mechanistic studies linking microvascular and neural biomarkers to cochlear pathology; and health-services research to determine cost-effectiveness of routine audiologic screening in diabetes clinics.
Conclusion
The recent PRISMA systematic review and meta-analysis synthesizing studies from 2019–2024 indicates that type 2 diabetes is associated with substantially higher odds of hearing loss (pooled OR 4.19), with greater impairment at high frequencies. Duration of diabetes (>10 years) and higher HbA1c levels were associated with higher prevalence and greater severity. Clinicians should be attentive to hearing health in adults with T2DM and consider integrating screening and referral into routine care, particularly for those with long-standing disease or poor glycaemic control. Continued prospective and interventional research is needed to clarify causality and define effective prevention strategies.
Funding and clinicaltrials.gov
Funding details and trial registrations were not extracted in this summary. For specific funding statements, conflicts of interest, and trial identifiers, consult the source article: Caballero-Borrego M, Andujar-Lara I. Otolaryngol Head Neck Surg. 2025;173(5):1041-1053.
References
1. Caballero-Borrego M, Andujar-Lara I. Type 2 Diabetes Mellitus and Hearing Loss: A PRISMA Systematic Review and Meta-Analysis. Otolaryngol Head Neck Surg. 2025 Nov;173(5):1041-1053. doi:10.1002/ohn.1346. PMID: 40922493; PMCID: PMC12574643.
2. Bainbridge KE, Hoffman HJ, Cowie CC. Diabetes and hearing impairment in the U.S. population. Ann Intern Med. 2008 Jul 1;149(1):1-10. doi:10.7326/0003-4819-149-1-200807010-00001.
3. World Health Organization. Deafness and hearing loss. WHO fact sheet. Published 2021. Available at: https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss
Thumbnail image prompt (AI friendly)
A middle-aged patient in a primary care clinic sitting at a small desk, a calibrated pure-tone audiogram machine visible with headset, a glucometer and HbA1c report on the table, clinician pointing to the audiogram; soft clinical lighting, neutral tones, photorealistic, focused on interaction and clinical tools.