Vitamin D is increasingly recognized for its critical role beyond skeletal health, impacting immune regulation, cellular growth, and cancer biology. Despite widespread vitamin D deficiency, particularly in populations practicing sun avoidance or living at higher latitudes, optimal serum levels remain insufficiently maintained globally. This systematic review evaluates the evidence supporting vitamin D’s protective effects against cancer incidence, progression, and mortality, and examines the challenges and implications for clinical practice.
Study Design
Utilizing PRISMA and PICOS frameworks, this systematic review synthesizes findings from randomized controlled trials (RCTs), observational, epidemiological, and mechanistic studies. Articles published between 1991 and 2025 were screened, focusing on adult populations with or without cancer, assessing interventions ranging from vitamin D supplementation, dietary intake, to ultraviolet B exposure, with endpoints encompassing cancer incidence, progression, and mortality.
Key Findings
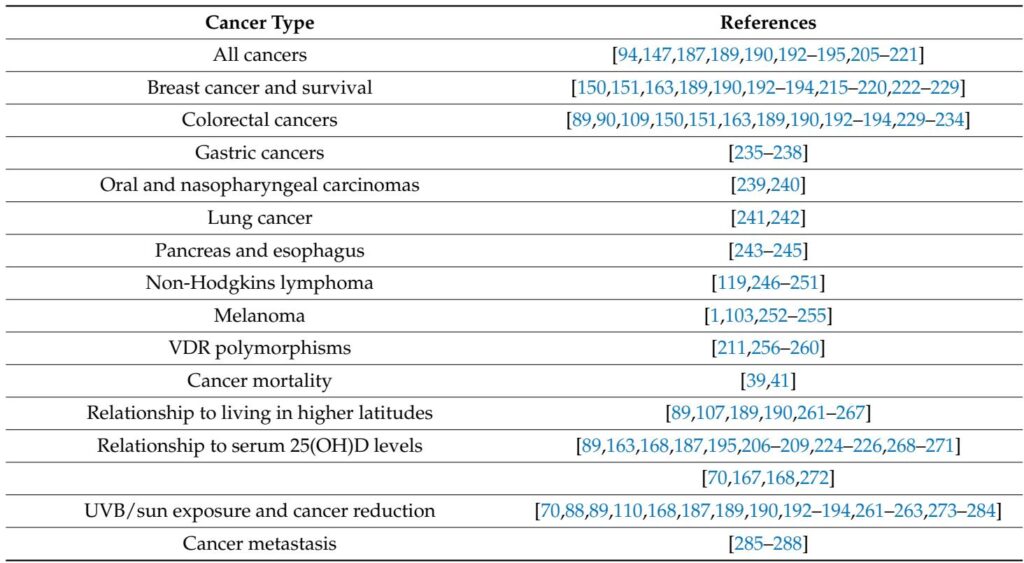
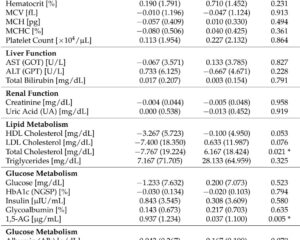
Vitamin D, primarily through its active form calcitriol (1,25(OH)2D), exerts multifaceted anticancer effects via genomic and non-genomic mechanisms. These include regulation of cell proliferation, promotion of differentiation and apoptosis, suppression of angiogenesis, and modulation of immune responses and inflammation. Epidemiological data consistently show an inverse correlation between serum 25-hydroxyvitamin D [25(OH)D] levels and the risk and mortality of various cancers such as breast, colorectal, gastric, pancreatic, and hematologic malignancies.
Maintaining serum 25(OH)D concentrations above 40 ng/mL (100 nmol/L) significantly reduces cancer incidence and improves survival, with optimal benefits often observed near 50–80 ng/mL. However, doses required to achieve such serum levels frequently exceed current government recommendations, especially in overweight and obese individuals.
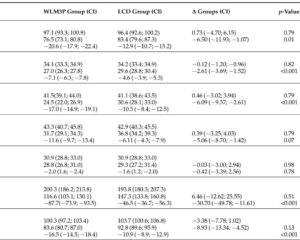
Recent large RCTs like the VITAL study have shown inconsistent benefits, primarily due to methodological design flaws, including enrolling vitamin D sufficient individuals, inadequate dosing regimens, short follow-up durations, and failure to measure or target optimal serum 25(OH)D levels. In contrast, well-designed RCTs and prospective cohort studies affirm vitamin D’s protective role, highlighting the necessity for precise study designs tailored for micronutrient research rather than classical pharmaceutical trial paradigms.
The role of combined vitamin D and calcium supplementation remains contentious, with some trials indicating reduced breast and colorectal cancer incidence among deficient populations, while others report negligible additive effects or even conflicting results.
Skin cancer risk, particularly melanoma, demonstrates complex interplay with vitamin D status and UV exposure. While excessive UV exposure can increase skin cancer risk, moderate sun exposure confers benefits through cutaneous vitamin D synthesis and may improve melanoma prognosis.
Genetic factors, including vitamin D receptor (VDR) polymorphisms and vitamin D-binding protein levels, further modulate individual responses to vitamin D and cancer risk.
Expert Commentary
The evidence validates vitamin D’s potential as a cost-effective, safe, and modifiable factor in cancer prevention and survival improvement. Clinical practice should incorporate strategies for maintaining serum 25(OH)D above 40 ng/mL, especially in high-risk groups. Importantly, clinical trials must be meticulously designed to consider baseline vitamin D status, dosing based on body weight or BMI, and enforce supplementation protocols achieving and sustaining therapeutic serum levels over appropriate durations.
Micronutrient research demands methodological innovations beyond traditional RCTs, including ecological studies, Mendelian randomization adjuncts, and advanced metabolic and genetic profiling. Furthermore, personalized supplementation and lifestyle modifications—including safe sun exposure—should form the backbone of preventive oncology guidelines.
Conclusion
Vitamin D sufficiency plays a critical role in reducing cancer incidence and mortality. Despite inconsistent RCT data due to design limitations, comprehensive evidence supports maintaining serum 25(OH)D levels in the 50–80 ng/mL range for optimal anticancer effects. Clinicians should proactively address vitamin D deficiency through personalized supplementation and encourage balanced sun exposure, integrating these measures into routine clinical guidelines. Future research must prioritize improved study designs and further elucidate the mechanistic underpinnings of vitamin D’s role in cancer biology.
Main References
Wimalawansa SJ. Vitamin D’s Impact on Cancer Incidence and Mortality: A Systematic Review. Nutrients. 2025 Jul 16;17(14):2333. doi: 10.3390/nu17142333. PMID: 40732958; PMCID: PMC12298439.
References
1. Wacker, M.; Holick, M.F. Sunlight and Vitamin D: A global perspective for health. Derm. Endocrinol. 2013;5:51–108.
2. Garland, C.F.; Garland, F.C.; Gorham, E.D.; et al. The role of vitamin D in cancer prevention. Am. J. Public Health. 2006;96(2):252–261.
3. Manson, J.E.; Cook, N.R.; Lee, I.M.; et al. Vitamin D supplements and prevention of cancer and cardiovascular disease. N Engl J Med. 2018;380:33–44.
4. Lappe, J.M.; Travers-Gustafson, D.; Davies, K.M.; Recker, R.R.; Heaney, R.P. Vitamin D and calcium supplementation reduces cancer risk: Results of a randomized trial. Am J Clin Nutr. 2007;85(6):1586–1591.
5. McCullough, M.L.; Zoltick, E.S.; Weinstein, S.J.; et al. Circulating vitamin D and colorectal cancer risk: An international pooling Project of 17 cohorts. J Natl Cancer Inst. 2019;111(2):158–169.
6. Grant, W.B.; Wimalawansa, S.J.; Pludowski, P.; et al. Vitamin D: Evidence-based health benefits and recommendations for population guidelines. Nutrients. 2025;17(2):277.
7. Heaney, R.P. Guidelines for optimizing design and analysis of clinical studies of nutrient effects. Nutr Rev. 2014;72(1):48–54.
8. Pilz, S.; Trummer, C.; Theiler-Schwetz, V.; et al. Critical appraisal of large vitamin D randomized controlled trials. Nutrients. 2022;14(2):303.
9. Grant, W.B. Sun exposure, vitamin D and cancer risk reduction. Eur J Cancer. 2013;49(14):2073–2075.
10. Holick, M.F. Vitamin D deficiency. N Engl J Med. 2007;357(3):266–281.