Highlight
– Excess adiposity is common in HFpEF patients, even among those with BMI below obesity thresholds.
– Obesity independently correlates with worsened cardiac remodeling, elevated pulmonary capillary wedge pressure (PCWP), and impaired exercise capacity.
– Insulin resistance (IR) and diabetes, while associated with obesity, do not independently worsen cardiac function or hemodynamics.
– These findings suggest diabetes primarily signals greater adiposity burden in HFpEF without directly exacerbating heart failure severity.
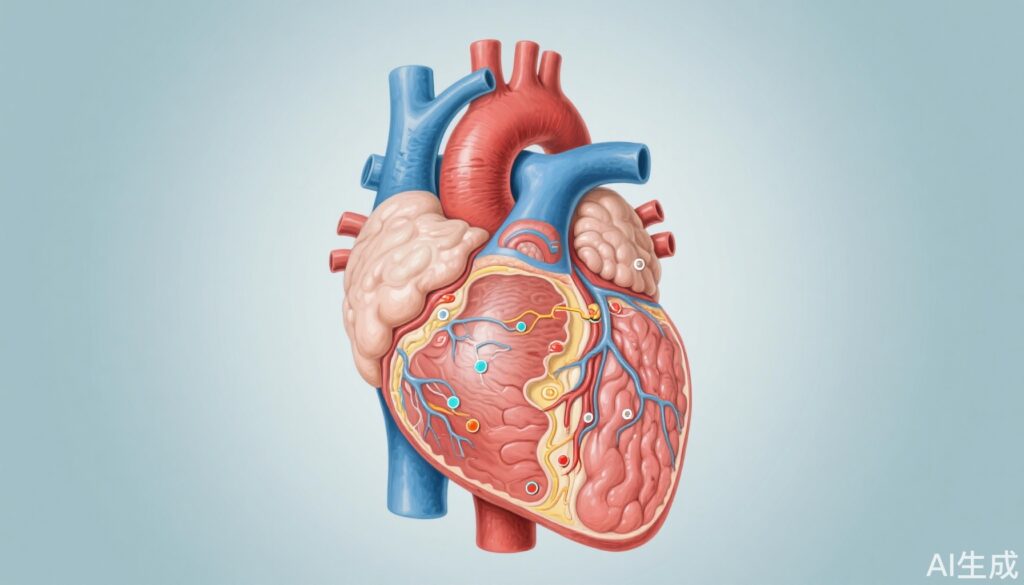
Study Background and Disease Burden
Heart failure with preserved ejection fraction (HFpEF) represents a significant and growing clinical challenge, encompassing nearly half of all heart failure cases globally. Obesity, insulin resistance (IR), and diabetes mellitus are prevalent comorbidities within this population and have been implicated as contributors to disease progression and prognosis. However, despite their frequent coexistence, the distinct contributions of adiposity and metabolic dysregulation to cardiac structural abnormalities and hemodynamic impairment in HFpEF have remained unclear. Understanding these independent effects is essential for devising targeted therapeutic strategies aimed at improving outcomes in this heterogenous syndrome.
Study Design
This investigation was a substudy within the Pulmonary Vascular Disease Phenomics Program (PVDOMICS; NCT02980887), enrolling 276 patients with HFpEF. Indices of adiposity including body mass index (BMI), bioimpedance-derived fat mass, and waist circumference were measured alongside insulin resistance quantified by the homeostasis-model assessment of IR (HOMA-IR). Patients were stratified according to obesity status (BMI 0 30 kg/m2), presence of IR (HOMA-IR 1 2.6), and diabetes diagnosis. Resting and exercise pulmonary capillary wedge pressure (PCWP) responses were assessed via invasive hemodynamics. Key endpoints included left heart remodeling parameters, exercise performance metrics, quality of life evaluations, and PCWP measures. Findings were validated in an independent HFpEF cohort of 254 patients.
Key Findings
Of the 276 HFpEF patients studied, 60% were obese by BMI criteria, and 89% demonstrated an elevated waist-to-height ratio indicative of excess central adiposity. Within the obese group, 69% exhibited insulin resistance, and 45% had diabetes. Notably, among non-obese patients (BMI <30 kg/m2), insulin resistance and diabetes prevalence were lower but still significant (40% and 25%, respectively; P < 0.0001 versus obesity phenotype).
Critically, the presence of insulin resistance or diabetes did not associate with greater left ventricular remodeling or elevated PCWP at rest or with exercise. In stark contrast, obesity—independent of insulin resistance—was linked with pronounced biventricular enlargement, reduced exercise capacity, poorer quality of life, and higher PCWP responses both at rest and during exertion (all P < 0.01).
Statistically, obesity increased resting and dynamic PCWP by approximately +4.4 mm Hg (95% CI: +2.5 to +6.4 mm Hg; P < 0.0001), a relationship that persisted even after adjusting for HOMA-IR (+4.7 mm Hg; 95% CI: +2.7 to +6.7 mm Hg; P < 0.0001). Higher values of fat mass, BMI, and waist circumference correlated robustly with PCWP elevations (P < 0.0009 for all). Conversely, HOMA-IR showed no significant association with PCWP (+0.01 mm Hg; 95% CI: -0.13 to +0.16 mm Hg; P = 0.84).
Substituting diabetes diagnosis in place of IR yielded comparable results. Validation in an independent HFpEF cohort confirmed that BMI, but not diabetes status, independently predicted elevated rest and exercise PCWP (+0.19 mm Hg per kg/m2; 95% CI: +0.11 to +0.27 mm Hg; P < 0.0001).
Expert Commentary
These data challenge the conventional perspective that insulin resistance and diabetes are primary drivers of hemodynamic impairment in HFpEF. Instead, the findings reposition excess adiposity as the pivotal factor mediating cardiac remodeling and elevated filling pressures. This distinction has crucial pathophysiological and therapeutic implications, as it emphasizes the potential benefit of interventions targeting fat mass reduction and metabolic health beyond glucose normalization.
The study’s strengths include robust invasive hemodynamic assessment at rest and exercise and confirmation in an independent cohort, enhancing the generalizability of results. However, potential limitations include observational design precluding causal inference and reliance on HOMA-IR, which, while validated, may not capture all nuances of metabolic dysfunction.
Biologically, excess adipose tissue generates systemic inflammation, neurohormonal activation, and mechanical cardiac loading, which likely contribute to observed remodeling and functional impairment more directly than insulin resistance alone. Further mechanistic studies are warranted to explore these pathways and to evaluate targeted cardiometabolic therapies in HFpEF patients with increased adiposity, including those with BMI below obesity thresholds.
Conclusion
The majority of patients with HFpEF harbor excess adiposity, which independently associates with adverse cardiac remodeling, worse hemodynamics, and impaired functional capacity, regardless of insulin resistance or diabetes status. Diabetes appears to predominantly reflect greater fat burden rather than exerting unique effects on heart failure severity. These insights underscore the importance of addressing adiposity and related metabolic factors in the management of HFpEF and highlight a clinical need to develop and assess therapies that effectively reduce adiposity and its cardiac consequences across the BMI spectrum.
References
Reddy YNV, Frantz RP, Hemnes AR, Hassoun PM, Horn E, Leopold JA, Rischard F, Rosenzweig EB, Hill NS, Erzurum SC, Beck GJ, Finet JE, Jellis CL, Mathai SC, Tang WHW, Borlaug BA; PVDOMICS Study Group. Disentangling the Impact of Adiposity From Insulin Resistance in Heart Failure With Preserved Ejection Fraction. J Am Coll Cardiol. 2025 May 13;85(18):1774-1788. doi: 10.1016/j.jacc.2025.03.530. PMID: 40335254.