Highlights
- Type II cryoglobulinemic vasculitis (CV) in primary Sjögren disease (pSD) is strongly linked to increased risk of non-Hodgkin lymphoma and mortality.
- Compared to other small-vessel vasculitides in pSD, type II cryoglobulinemic vasculitis is associated with more severe visceral involvement, including renal and peripheral nervous system complications.
- Rituximab-based therapy may reduce lymphoma risk in this high-risk group, though mortality remains high.
- Findings underscore the need for targeted monitoring and management strategies for these patients.
Study Background and Disease Burden
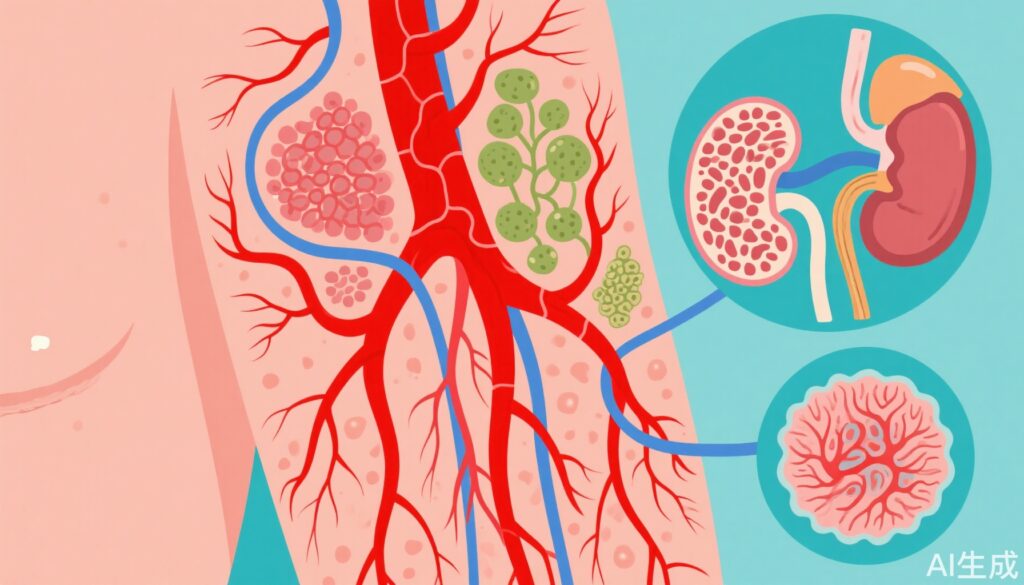
Primary Sjögren disease (pSD) is a systemic autoimmune disorder predominantly affecting exocrine glands, leading to sicca symptoms and a spectrum of extraglandular manifestations. A significant complication in pSD is small-vessel vasculitis, particularly cryoglobulinemic vasculitis (CV), which arises from circulating immune complexes that precipitate at low temperatures. Among the different types, type II cryoglobulinemia, characterized by mixed monoclonal and polyclonal immunoglobulins, is clinically significant due to its strong association with lymphoproliferative disorders and organ involvement. The identification of predictive markers for poor outcomes, especially lymphoma and mortality, is a critical unmet need in managing pSD.
Study Design
This French multicenter retrospective cohort study analyzed 54 patients with pSD and cutaneous vasculitis (CV), drawn from three Parisian pathology departments and a national case registry, with a median age of 42 years and a female predominance (91%). Patients were diagnosed with CV between 2011 and 2021. Among them, 29 (57%) had cryoglobulinemic vasculitis (24 of which were type II), while 15 (28%) exhibited hypergammaglobulinemic vasculitis. Data collection and analysis occurred between March 2023 and March 2025.
To evaluate the prognostic impact of CV subtypes, patients were matched in a 1:2 ratio to 108 controls with pSD but without CV, sourced from the French ASSESS cohort. The primary outcomes assessed were the incidence of lymphoma and all-cause mortality.
Key Findings
1. Lymphoma Risk and Mortality: The study demonstrated that patients with pSD and any form of cutaneous vasculitis had a higher incidence of lymphoma compared to those without CV (13% vs 4%, P = .04). Notably, type II cryoglobulinemic vasculitis conferred particularly high risk: 21% developed lymphoma versus 0% among those with other small-vessel vasculitides (P = .02). Mortality was also markedly higher in the type II group (29% vs 0%, P = .02).
2. Magnitude of Risk: The composite risk for death or non-Hodgkin lymphoma was nearly sevenfold higher in type II cryoglobulinemic vasculitis compared with other CV types (HR, 6.8; P = .005). This finding underscores the unique pathogenicity of type II cryoglobulinemic processes in pSD.
3. Clinical Features and Organ Involvement: Patients with type II cryoglobulinemic vasculitis were significantly more likely to present with:
- Subacute cutaneous lupus (21% vs 0%, P = .02)
- Renal involvement (29% vs 4%, P = .02)
- Peripheral nervous system involvement (63% vs 12%, P < .001)
These findings indicate that type II cryoglobulinemic vasculitis in pSD is not only a cutaneous process but also a marker for severe systemic disease.
4. Therapeutic Implications: Among 24 patients with type II cryoglobulinemic vasculitis, half received first-line rituximab-based therapy. The incidence of non-Hodgkin lymphoma was lower in the rituximab group (8%) than among those treated with other regimens (25%). However, mortality rates were similar (33% in rituximab vs 25% non-rituximab), suggesting persistent unmet need for improved interventions.
Expert Commentary
The authors conclude that, in contrast to other vasculitic subtypes, only type II cryoglobulinemic vasculitis in pSD is associated with severe visceral involvement and a markedly worse prognosis. This observation aligns with prior studies linking mixed cryoglobulinemia to lymphoproliferative evolution in autoimmune settings. The sevenfold increase in combined mortality and lymphoma risk highlights a critical subset of pSD patients requiring intensive surveillance.
Current international guidelines recommend vigilant monitoring for lymphoproliferative complications in pSD with cryoglobulinemia, but the present study provides robust, real-world evidence for stratified risk. The partial risk reduction with rituximab-based therapy suggests a possible disease-modifying effect, but the persistently high mortality underscores the need for earlier identification and perhaps adjunctive or novel therapies.
Limitations include the retrospective design, limited sample size, and potential referral bias inherent in tertiary center data. Nevertheless, the multicenter approach and control matching strengthen the validity of the findings.
Conclusion
Type II cryoglobulinemic vasculitis identifies a high-risk phenotype among patients with primary Sjögren disease, characterized by increased risk for lymphoma, severe organ involvement, and early mortality. Clinicians should maintain a high index of suspicion and implement targeted surveillance in this subgroup. Further research is needed to elucidate optimal therapeutic strategies and to explore potential biomarkers for earlier risk detection.
References
- Paul Breillat, Véronique Le Guern, Thomas d’Humières, et al. Cutaneous Vasculitis in Primary Sjögren Disease. JAMA Dermatol. Published Online: August 6, 2025. doi:10.1001/jamadermatol.2025.2665
- Mariette X, Criswell LA. Primary Sjögren’s Syndrome. N Engl J Med. 2018;378(10):931-939. doi:10.1056/NEJMra1704096
- Retamozo S, et al. Cryoglobulinemic vasculitis in systemic autoimmune diseases. J Autoimmun. 2012;39(3):200-207. doi:10.1016/j.jaut.2012.05.014