Highlight
- Microaxial flow pump therapy significantly reduces 180-day mortality in patients with infarct-related cardiogenic shock who present with systolic blood pressure (SBP) below 82 mm Hg.
- Patients with higher SBP at randomization do not derive notable survival benefit from this therapy compared to standard care alone.
- Early SBP measurement can help identify the patient subgroup most likely to benefit from microaxial pump support, aiding clinical decision-making.
Study Background and Disease Burden
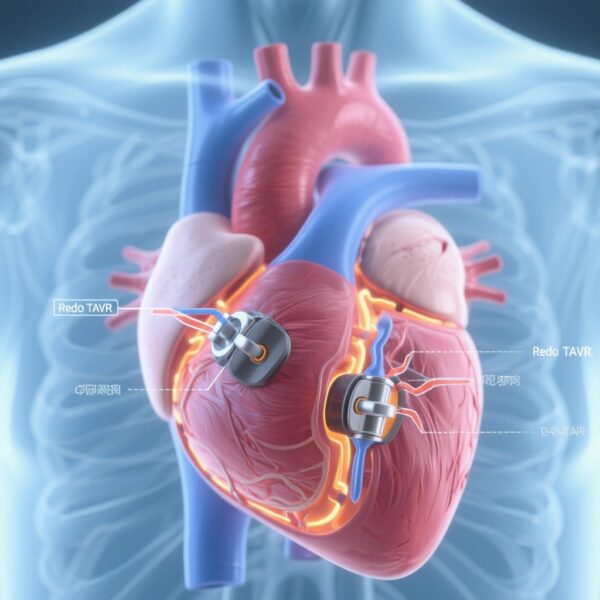
Cardiogenic shock (CS) secondary to ST-segment elevation myocardial infarction (STEMI) remains a leading cause of in-hospital mortality despite advances in reperfusion and supportive care. This condition is characterized by profound cardiac pump failure resulting in inadequate tissue perfusion, hypotension, and multi-organ dysfunction. Mechanical circulatory support devices, such as microaxial flow pumps, have emerged as adjunctive treatment options aimed at improving hemodynamics and outcomes. However, these devices carry risks including bleeding, vascular injury, and hemolysis. Moreover, the survival benefit of microaxial flow pump therapy may not be uniform across all patients with infarct-related CS, and identifying subgroups deriving maximal benefit remains an unmet clinical need.
Systolic blood pressure (SBP) on presentation, a sensitive indicator of shock severity, has been hypothesized to modify the effect of mechanical circulatory support on survival outcomes. Understanding the interplay between SBP and therapeutic benefit is critical to optimize patient selection, maximize benefit, and minimize procedure-related risks.
Study Design
This investigation is a post hoc analysis drawn from the Danish-German (DanGer) Shock trial, an open-label randomized clinical trial conducted from 2013 to 2023 involving 355 adult patients with STEMI complicated by cardiogenic shock. Enrollment occurred at 14 tertiary invasive cardiac centers across Denmark, Germany, and the United Kingdom. Patients were randomized to receive either microaxial flow pump therapy plus standard care or standard care alone. The primary endpoint analyzed was all-cause mortality at 180 days. Systolic blood pressure was measured at randomization and analyzed as a potential modifier of treatment effect. Statistical methods included dichotomized regression analysis, Kaplan-Meier survival curves, and spline regression to evaluate interactions between SBP levels and mortality outcomes.
Key Findings
Of the 355 patients randomized, systolic blood pressure at randomization was available for 351 (median age 69 years, interquartile range 59–76; 79% male). The analysis identified a clear interaction between SBP and the survival benefit of microaxial flow pump therapy. Patients with SBP below 82 mm Hg at randomization experienced a statistically significant reduction in 180-day mortality when treated with microaxial flow pump therapy compared to standard care alone (odds ratio [OR] 0.34; 95% CI 0.18–0.63; P < .001). Conversely, in patients with SBP above 82 mm Hg, no significant survival advantage was seen with microaxial pump use (OR 0.96; 95% CI 0.53–1.70; P = .90).
Further supporting these findings, Kaplan-Meier survival analyses and spline regression demonstrated a significant interaction between SBP and treatment effect (P for interaction = .02) alongside evidence of non-linear association (P for nonlinearity = .01), underscoring a threshold effect at lower SBP levels.
Importantly, these results suggest that the most hypotensive patients—those at greatest immediate hemodynamic risk—derive the largest survival benefit from early mechanical circulatory support via microaxial pumps. This selective benefit offers an opportunity to tailor therapy more precisely, balancing potential survival gains against procedure-related risks.
Expert Commentary
The findings from this post hoc DanGer Shock analysis contribute important nuance to clinical decision-making in infarct-related cardiogenic shock. While randomized controlled trials have previously shown overall mortality benefit with microaxial flow pumps, this analysis advances our understanding by highlighting SBP as a key clinical parameter that modifies treatment responsiveness.
Physiologically, lower SBP at presentation reflects more severe circulatory failure, where enhanced mechanical support to maintain end-organ perfusion could be particularly lifesaving. Conversely, patients with higher SBP may maintain sufficiently adequate perfusion such that the risks of invasive pump support are not outweighed by survival benefits. These insights align with clinical observations that benefit-risk assessment must be individualized in cardiogenic shock treatment.
Clinicians should consider incorporating early SBP assessment as a stratification tool when deciding on microaxial pump implementation. However, as these are post hoc and hypothesis-generating findings, prospective validation is needed. Limitations include potential residual confounding and the open-label nature of the original trial. Further research might explore integration with other clinical and biomarker indicators to refine patient selection.
Conclusion
Microaxial flow pump therapy confers a significant survival benefit in patients with infarct-related cardiogenic shock who present with markedly low systolic blood pressure (< 82 mm Hg). Early SBP measurement is a promising biomarker for identifying patients most likely to gain from this mechanical circulatory support, helping clinicians optimize therapeutic decisions and improve outcomes. These results underscore the importance of personalized treatment strategies in cardiogenic shock and warrant further prospective investigation to confirm SBP-guided patient selection protocols.
References
Mikkelsen AD, Beske RP, Jensen LO, et al; DanGer Shock Investigators. Systolic Blood Pressure and Microaxial Flow Pump-Associated Survival in Infarct-Related Cardiogenic Shock: A Post Hoc Analysis of the DanGer Shock Randomized Clinical Trial. JAMA Cardiol. 2025 Aug 30:e253337. doi:10.1001/jamacardio.2025.3337. Epub ahead of print. PMID: 40884241; PMCID: PMC12398770.
Thiele H, Zeymer U, Neumann FJ, et al; CULPRIT-SHOCK Investigators. Invasive management of acute myocardial infarction complicated by cardiogenic shock. N Engl J Med. 2012;367(9): 893-904.
Burkhoff D, Naidu SS. The science behind percutaneous hemodynamic support: a review and comparison of devices. Circ Heart Fail. 2012;5(3): 276-286.