Study Background and Disease Burden
Nasopharyngeal carcinoma (NPC) is a malignancy originating in the epithelial lining of the nasopharynx, showing a high prevalence in East and Southeast Asia. Locoregionally advanced NPC (LA-NPC), corresponding to stages III and IVA per the American Joint Committee on Cancer (AJCC) staging system, presents significant management challenges due to its aggressive nature and risk of both local recurrence and distant metastasis. The current standard of care involves induction chemotherapy (IC) followed by concurrent chemoradiotherapy (CCRT), a regimen that has improved survival outcomes significantly. However, the CCRT phase is frequently accompanied by substantial acute toxic effects, particularly severe mucositis, which complicates treatment adherence and quality of life.
Given these challenges, there has been clinical interest in exploring alternative therapeutic approaches that maintain efficacy but reduce toxicity. Sequential chemoradiotherapy (SCRT), consisting of IC followed by radiotherapy alone and then adjuvant chemotherapy (AC), may potentially reduce acute toxic effects during radiotherapy by omitting concurrent chemotherapy. Nevertheless, robust data evaluating whether SCRT can safely and effectively replace IC plus CCRT have been lacking.
Study Design
This was a multicenter, open-label, phase 3 noninferiority randomized clinical trial conducted across six centers in China from January 2018 to September 2021. The trial enrolled 420 patients aged 18 to 65 years with newly diagnosed stage III/IVA nasopharyngeal carcinoma. Patients were randomized 1:1 into two treatment arms:
– SCRT group: Two cycles of induction chemotherapy using gemcitabine and cisplatin (GP regimen), followed by radiotherapy alone, then two cycles of adjuvant chemotherapy with the same GP regimen.
– IC plus CCRT group: Two cycles of induction chemotherapy (GP regimen) followed by radiotherapy concurrent with weekly cisplatin (30 mg/m2).
The primary endpoints were 3-year failure-free survival (FFS) with a noninferiority margin set at a 10% difference (hazard ratio [HR] less than 1.6), and incidence of grade 3 or higher acute mucositis during radiotherapy. Secondary endpoints included overall survival, locoregional FFS, distant FFS, response rate, and acute and late toxic effects.
Key Findings
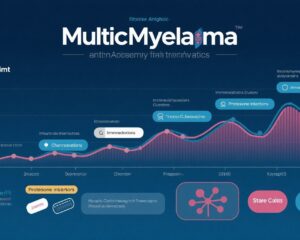
Among the 420 enrolled patients (median age 48 years, 25.5% female), 210 were assigned to each arm. The median follow-up was approximately 50 months. In the intention-to-treat analysis, the 3-year FFS was 83.7% (95% CI, 78.6–88.8) for the SCRT arm versus 79.5% (95% CI, 74.0–85.0) for the IC plus CCRT arm, with a hazard ratio of 0.77 (95% CI, 0.50–1.19; P=0.24). The upper bound of the 95% confidence interval was below the predefined noninferiority margin, indicating that SCRT was noninferior to the standard regimen.
Importantly, the SCRT group experienced significantly fewer grade 3 or higher acute nonhematological toxic effects during radiotherapy:
– Acute mucositis occurred in 29.0% (61/210) of SCRT patients versus 41.9% (88/210) in the IC plus CCRT group (P < .001).
– Nausea was reported in 9.5% versus 18.1% (P = .01).
– Vomiting occurred in 3.8% versus 9.5% (P = .02).
There were no statistically significant differences in late toxic effects between the two arms.
Expert Commentary
This trial provides important evidence supporting SCRT as a viable alternative to the current standard of IC plus CCRT for locoregionally advanced nasopharyngeal carcinoma. By decoupling chemotherapy from radiotherapy and administering adjuvant chemotherapy after radiation, SCRT reduces the intensity of acute toxicity, particularly mucositis, a common and debilitating side effect that often limits treatment completion and results in hospitalizations.
The noninferiority in 3-year FFS suggests that omitting concurrent chemotherapy during radiotherapy does not compromise disease control in the context of adequate induction and adjuvant chemotherapy. This finding aligns with the evolving understanding of the synergistic but also additive toxicities of concurrent chemoradiation.
Limitations include the open-label design and the geographical confinement to centers in China, which may limit generalizability to populations with different genetic backgrounds or healthcare infrastructures. Further studies could validate quality of life outcomes and long-term survival beyond 3 years.
Conclusion
The results from this prospective, phase 3 randomized trial demonstrate that sequential chemoradiotherapy (induction chemotherapy followed by radiotherapy and then adjuvant chemotherapy) is noninferior to the standard induction chemotherapy plus concurrent chemoradiotherapy in terms of 3-year failure-free survival in patients with locoregionally advanced nasopharyngeal carcinoma. Crucially, SCRT significantly reduces the incidence of severe acute nonhematological toxicities such as mucositis, nausea, and vomiting during treatment.
These findings offer a potentially safer alternative treatment approach that may improve patient tolerability and compliance without compromising efficacy, addressing a significant clinical unmet need. Incorporating SCRT into treatment guidelines warrants consideration after validation in diverse populations and further assessment of quality of life and long-term outcomes.
References
1. Xue F, Ou D, Xie C, et al. Sequential vs Induction Plus Concurrent Chemoradiotherapy in Nasopharyngeal Carcinoma: A Randomized Clinical Trial. JAMA Oncol. 2025 Jul 24:e252191. doi:10.1001/jamaoncol.2025.2191.
2. Lee AW, Ng WT, Chan LL, et al. Management of Nasopharyngeal Carcinoma: Current Practice and Future Perspective. J Clin Oncol. 2015;33(29):3356-3364. doi:10.1200/JCO.2015.62.2427
3. Chen L, Hu CS, Chen XZ, et al. Concurrent Chemoradiotherapy in Locoregionally Advanced Nasopharyngeal Carcinoma: A Nine-Year Retrospective Study. Int J Radiat Oncol Biol Phys. 2020;106(3):524-531. doi:10.1016/j.ijrobp.2019.11.024