Highlight
– The ventricular septum (VS) curvature ratio measured on CTPA strongly predicted 30‑day clinical deterioration in normotensive acute pulmonary embolism (PE) in a large prospective multicentre cohort (n=3,310).
– Patients with VS curvature ratios ≥1.90 or with straight/bowed septa toward the left ventricle had markedly higher odds of deterioration (OR ≈23) compared with those with ratios <1.60.
– The VS curvature ratio demonstrated good discrimination (AUC 0.83–0.84) across centres, suggesting reproducibility and potential for integration into early triage pathways for normotensive PE.
Background
Acute pulmonary embolism is a common and potentially life‑threatening cardiovascular emergency. While haemodynamically unstable patients are treated urgently as high risk, most patients present normotensive and have highly variable clinical courses. Early identification of the subset of normotensive patients who will deteriorate (require escalation to thrombolysis, vasopressors, mechanical ventilation, or experience death) remains a major unmet need in triage and management.
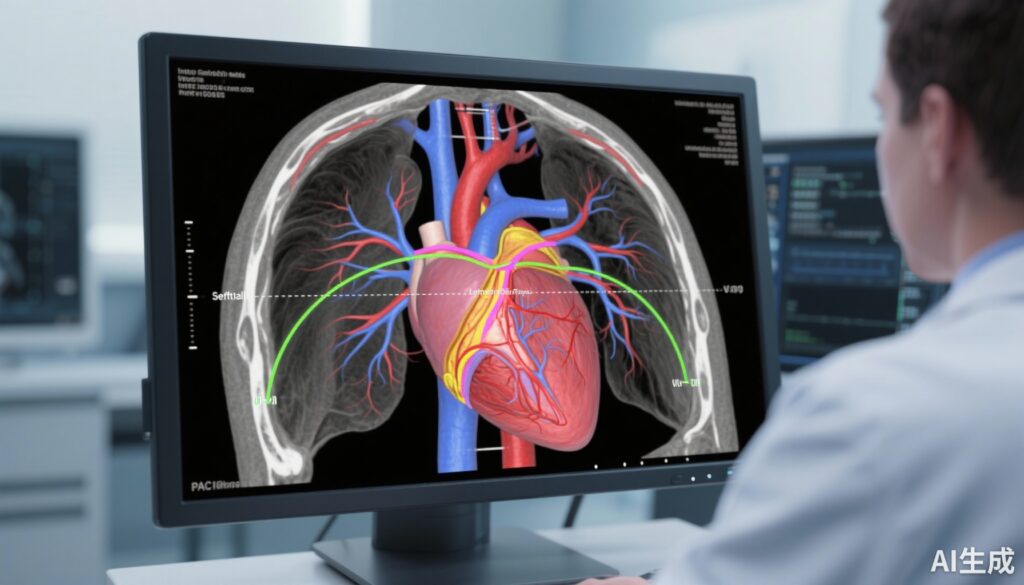
Computed tomography pulmonary angiography (CTPA) is routinely obtained at diagnosis and provides anatomic and indirect functional information about right ventricular (RV) strain. Established CTPA markers such as RV/LV diameter ratio and interventricular septal bowing have been associated with adverse outcomes, but qualitative descriptors and single linear measurements are imperfect and variably reproducible. The ventricular septum curvature ratio is a quantitative metric that compares the curvature radii of the interventricular septum and the left ventricular free wall on axial CTPA slices. Gao and colleagues prospectively evaluated whether this novel imaging marker improves prediction of clinical deterioration among normotensive patients with acute PE.
Study Design
This was a prospective, multicentre cohort study conducted across five centres in China from January 2021 to June 2024 (ClinicalTrials.gov NCT05098769). Key features:
- Population: Adults with acute PE who were normotensive at presentation (systolic blood pressure ≥90 mmHg), enrolled consecutively across participating centres.
- Index test: Ventricular septum and left ventricular (LV) free‑wall curvature radii measured on standard axial CTPA images; the VS curvature ratio (VS radius / LV free‑wall radius) was calculated. Septal configuration was categorized into four groups: VS bowing to the RV with curvature ratio <1.60; 1.60–<1.90; ≥1.90; and a fourth group with VS straight or bowing to the LV.
- Endpoint: Occurrence of a clinical deterioration event within 30 days of admission (composite of haemodynamic collapse, need for thrombolysis/interventional therapy, escalation to mechanical ventilation, use of vasopressors, or death).
- Analysis: Hierarchical logistic regression adjusted for centre and relevant clinical covariates; discriminatory performance estimated by area under the receiver operating characteristic curve (AUC). Internal validation included comparison across local and non‑local centres.
Key Findings
Population and outcomes
Among 3,310 normotensive patients with acute PE, 272 (8.2%) experienced clinical deterioration within 30 days. The primary analytic cohort included 3,030 patients from three local centres for detailed septal categorization; an external-like validation cohort comprised 280 patients from two other centres.
VS curvature ratio categories and risk
Using a VS curvature ratio <1.60 as the reference group, the study found large and statistically significant increases in odds of 30‑day deterioration for patients with more abnormal septal curvature:
- VS curvature ratio ≥1.90: OR 22.94 (p < 0.05)
- VS straight or bowing to the LV: OR 22.95 (p < 0.05)
These effect sizes are substantial, indicating that patients whose septal configuration is markedly abnormal by this metric have a multilateral-fold higher adjusted risk of clinical deterioration compared with those with lower ratios.
Discriminatory performance
The VS curvature ratio demonstrated strong discrimination for the 30‑day deterioration endpoint, with AUCs of 0.83 in the three-index centres and 0.84 in the two non‑local centres. These AUC values indicate good-to-excellent model discrimination and suggest that the marker retains performance across different imaging populations and practice settings.
Reproducibility and practical implementation
The study reports consistent results across participating centres and a clear categorical thresholding approach that could be translatable into routine CTPA reading. The metric relies on anatomical measurements on commonly acquired axial slices, which could be integrated into PACS measurement tools or automated image-processing pipelines.
Safety and secondary observations
No imaging-related harms were reported; the study focused on prognostic discrimination rather than therapeutic interventions. The authors note that adding the VS curvature ratio to existing clinical and imaging risk stratification frameworks may refine decision-making about early monitoring intensity, right‑sided haemodynamic surveillance, and consideration for escalated therapy in select normotensive patients.
Expert Commentary
The findings by Gao et al. introduce a promising quantitative imaging biomarker that operationalizes septal morphology into a continuous and thresholdable metric. Biological plausibility is strong: acute RV pressure overload leads to septal flattening and leftward bowing; comparing septal curvature to the left ventricular free wall normalizes for patient-specific cardiac size and image scaling, potentially improving robustness relative to single linear diameters.
Strengths
- Large multicentre prospective design with a clinically relevant composite endpoint focused on early deterioration.
- Clear, reproducible measurement technique amenable to standard PACS tools or automation.
- Demonstrated discrimination across centres, suggesting external validity.
Limitations
- Although prospective and multicentre, the cohort was geographically limited to centres in China; applicability to other healthcare systems, imaging protocols, and ethnic groups requires confirmation.
- The authors present categorical cutpoints, but threshold selection may benefit from further refinement using decision-curve analysis to quantify clinical net benefit when incorporated into triage algorithms.
- Comparative performance versus established clinical risk tools (PESI/sPESI) and other imaging markers (RV/LV diameter ratio, pulmonary artery obstruction index) requires direct head‑to‑head evaluation; the report focused primarily on the VS curvature ratio’s standalone discrimination.
- Potential measurement variability across observers, slice selection, or CT acquisition parameters was not fully characterized; formal inter‑ and intraobserver reproducibility statistics (intraclass correlation coefficients) should be reported in subsequent work.
Clinical implications and next steps
If validated externally and integrated into routine reporting, the VS curvature ratio could help clinicians identify normotensive PE patients who warrant closer observation, earlier echocardiography, intensive monitoring, or expedited consideration for reperfusion therapies. Prospective studies comparing management strategies guided by this marker versus standard care are needed to determine whether its use improves patient‑centred outcomes and is cost‑effective.
Conclusion
This large prospective multicentre study demonstrates that a quantitative ventricular septum curvature ratio measured on routine CTPA images is a strong predictor of 30‑day clinical deterioration in normotensive acute pulmonary embolism. With AUCs around 0.83–0.84 and very high odds ratios for the most abnormal categories, the metric shows promise as an adjunct to conventional clinical and imaging risk stratification.
Before broad adoption, external validation across diverse populations, standardization of measurement protocols, assessment of reproducibility, and trials assessing the impact of VS curvature ratio–guided management on clinical outcomes are advisable. Nonetheless, the approach is appealing because it leverages routinely acquired imaging and provides a biologically plausible, quantitative readout that could be integrated into clinical workflows or automated imaging analytics.
Funding and ClinicalTrials.gov
The study is registered at ClinicalTrials.gov (Identifier: NCT05098769; registered October 16, 2021). Funding statements reported by the authors are included in the original publication (Gao et al., Crit Care 2025).
References
1. Gao Y, Gu Z, Wei X, Wei S, Liu Y, Zhan S, Yang J, Qi C, Qi S, Wang M, Jia D. Ventricular septum curvature ratio: a novel imaging marker to predict clinical deterioration in normotensive acute pulmonary embolism. Crit Care. 2025 Oct 31;29(1):463. doi: 10.1186/s13054-025-05708-w. PMID: 41174707; PMCID: PMC12577156.
2. Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing GJ, Harjola VP, Huisman MV, Humbert M, Jennings C, Jiménez D, Leclercq C, Lankeit M, Lorusso R, Mazzolai L, Meneveau N, Ni Ainle F, Perrier A, Prandoni P, Pumpalova Y, Righini M, Sors H, Torbicki A, Zompatori M; ESC Scientific Document Group. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J. 2020 Jan 21;41(4):543-603.
Author note
This article synthesizes and interprets the primary findings of Gao et al. (2025) and places them in the context of current PE risk stratification practice. Readers are encouraged to consult the original publication for detailed methodology, complete statistical models, and supplementary materials.