Highlight
This study from Asan Medical Center provides compelling evidence that decreased retinal parafoveal vascular density (PFVD), as assessed by optical coherence tomography angiography (OCTA), strongly associates with subclinical coronary artery disease (CAD) in asymptomatic individuals. The superficial capillary plexus (SCP) density offers superior predictive performance for coronary atherosclerotic burden compared to the deep capillary plexus (DCP). Incorporating PFVD metrics alongside traditional cardiovascular risk factors improves identification of obstructive and severe CAD, offering a promising adjunctive biomarker for early detection and risk stratification.
Study Background and Disease Burden
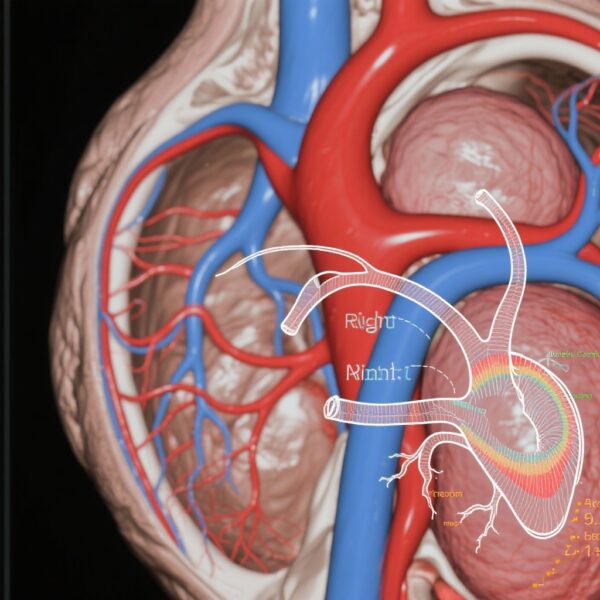
Coronary artery disease remains a leading cause of morbidity and mortality worldwide, often progressing silently before clinically manifesting as myocardial infarction or sudden cardiac death. Early detection of subclinical coronary atherosclerosis can enable preventive interventions but relies primarily on imaging modalities like coronary computed tomography angiography (CTA) or invasive coronary angiography, which have limitations including cost, radiation exposure, and accessibility.
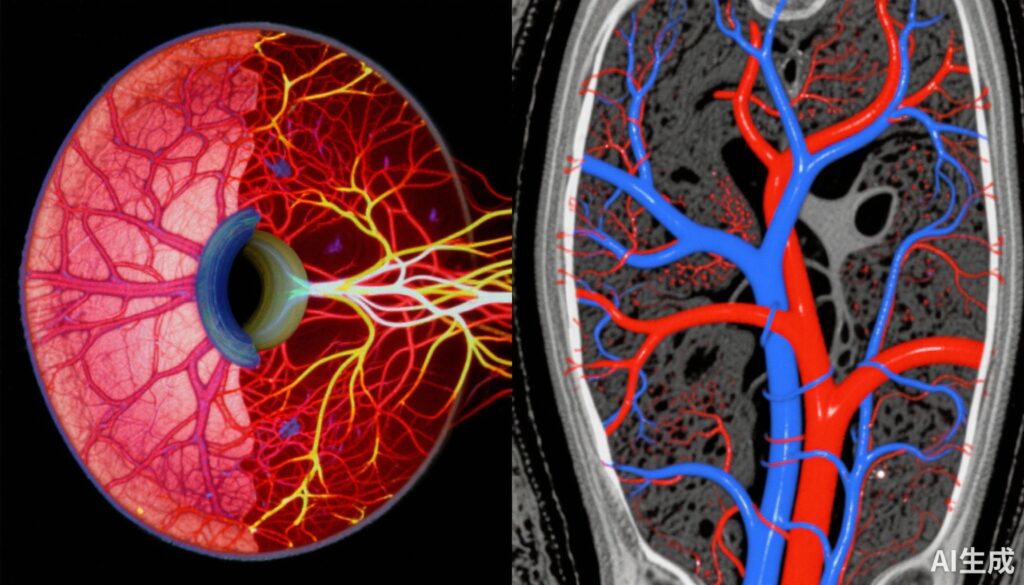
The retina is a unique window into systemic microvascular health, sharing embryologic and physiological properties with cerebral and coronary vasculature. Optical coherence tomography angiography (OCTA) is a noninvasive imaging technique that maps retinal microvascular networks, quantifying vascular density without dye injection. Systemic diseases including hypertension, diabetes, and stroke have demonstrated concurrent alterations in retinal microvasculature, but whether OCTA parameters can reliably serve as surrogates for coronary atherosclerosis has remained uncertain.
Study Design
This cross-sectional cohort study enrolled 1286 asymptomatic adults with elevated cardiovascular risk who self-referred to a health screening program at Asan Medical Center, Seoul, between October 2015 and December 2020. Participants underwent coronary CTA to assess coronary artery calcium score (CACS), presence and subtype of coronary plaques, obstructive coronary artery disease (CAD), and severity indices such as segment stenosis score (SSS) and segment involvement score (SIS). Ophthalmic evaluation included OCTA imaging to quantify superficial and deep parafoveal vascular density (PFVD) in the retinal capillary plexuses.
The primary objective was to evaluate associations between retinal PFVD parameters and coronary atherosclerosis metrics, adjusting for traditional cardiovascular risk factors including age, sex, smoking, hypertension, diabetes, and lipid profiles. Data analysis spanned January 2021 to May 2025.
Key Findings
Analysis included 1286 eyes from 1286 participants (mean age 64.2 ± 9.9 years; 37.5% female). Coronary artery calcium scores, plaque prevalence, and CAD severity significantly increased across decreasing quartiles of both superficial and deep PFVD.
When examining continuous measures, OCTA metrics from the superficial capillary plexus exhibited the strongest inverse correlations with CACS, number of affected coronary vessels, SSS, and SIS. Participants in the lowest quartile of superficial PFVD showed markedly elevated adjusted odds for obstructive CAD (aOR 2.91; 95% CI 1.83–4.73), severe CAD (aOR 3.30; 95% CI 1.55–7.91), and higher stenosis scores compared to those in the highest quartile. Similar but less pronounced associations were observed for deep PFVD.
Importantly, modeling PFVD as a continuous variable revealed a linear inverse relationship with CAD burden, supporting dose-dependent predictive potential. Incorporation of PFVD into multivariable risk prediction models enhanced discrimination for severe and obstructive CAD, reflected by increased areas under the curve (AUC ranging 0.77–0.79), with the superficial plexus metrics outperforming deep plexus metrics.
Expert Commentary
This study advances the concept of retinal vascular imaging as a surrogate marker for systemic atherosclerotic disease. The significant association between reduced retinal microvascular density and coronary atherosclerosis highlights shared pathophysiological mechanisms such as microvascular endothelial dysfunction, inflammation, and vascular remodeling.
While the cross-sectional design precludes causal inference, findings are robust across multiple coronary disease indices and adjust for prominent confounders. Future prospective studies are warranted to evaluate longitudinal predictive utility and whether retinal OCTA changes precede clinical CAD events.
The superior performance of superficial capillary plexus density over deep plexus metrics may reflect differential vulnerability of retinal microvascular layers or signal quality variations. Operator-independent, reproducible OCTA measurements enhance clinical feasibility.
However, generalizability is limited to an Asian population with elevated vascular risk attending health screening, and external validation is needed. OCTA’s accessibility and cost barriers outside ophthalmology clinics also merit consideration in broader cardiovascular screening paradigms.
Conclusion
Reduced retinal parafoveal vascular density measured by OCTA independently associates with subclinical coronary atherosclerosis in asymptomatic individuals at increased cardiovascular risk. This noninvasive retinal imaging marker complements traditional risk factors to improve identification of subclinical CAD burden, with potential utility in guiding targeted coronary evaluation and preventive strategies. Integrating retinal microvascular assessment into cardiovascular risk stratification represents a promising frontier bridging ophthalmology and cardiology.
Further longitudinal and multicenter studies are needed to validate these findings across diverse populations, explore mechanistic pathways, and establish standardized OCTA protocols for cardiovascular risk screening.
References
Yang JM, Yang DH, Lee SW, Kwak J, Lee Y, Kim YJ, Lee JY, Sung KR, Yoon YH. Subclinical Coronary Atherosclerosis and Retinal Optical Coherence Tomography Angiography. JAMA Cardiol. 2025 Sep 17:e253036. doi: 10.1001/jamacardio.2025.3036. Epub ahead of print. PMID: 40960791; PMCID: PMC12444650.
Patton N, Aslam T, MacGillivray T, Pattie A, Deary IJ, Dhillon B. Retinal vascular image analysis as a potential screening tool for cerebrovascular disease: a rationale based on homology between cerebral and retinal microvasculatures. J Anat. 2005 Jul;206(4):319-48. doi: 10.1111/j.1469-7580.2005.00409.x.
Tu W, Li J, Huang Y, et al. Correlation between Retinal Microvascular Abnormalities and Coronary Artery Disease: A Systematic Review and Meta-Analysis. J Am Heart Assoc. 2020;9(4):e014138. doi:10.1161/JAHA.119.014138.
de Carlo TE, Romano A, Waheed NK, Duker JS. A review of optical coherence tomography angiography (OCTA). Int J Retina Vitreous. 2015 Sep 7;1:5. doi: 10.1186/s40942-015-0005-8.