Highlight
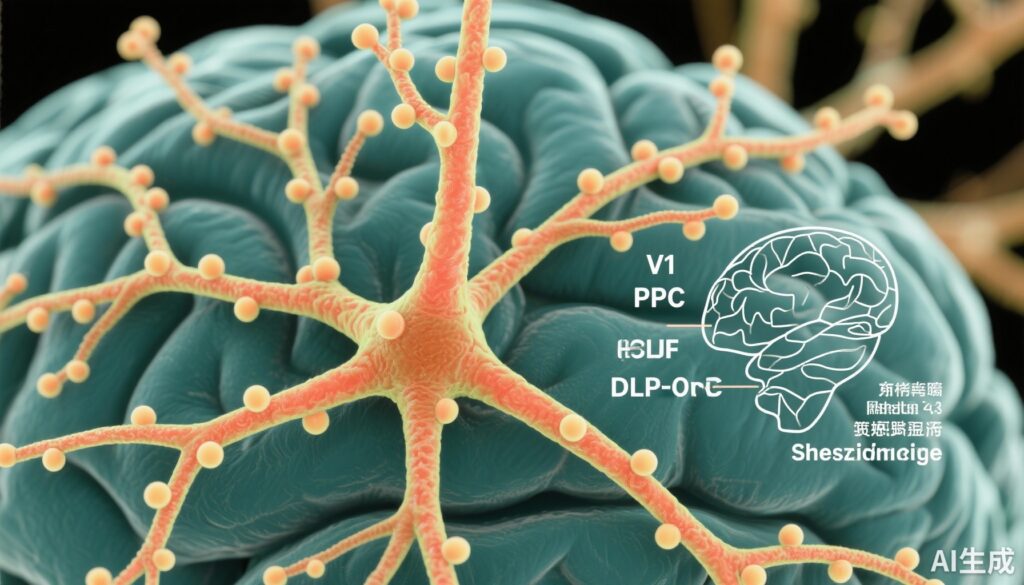
- Schizophrenia (SZ) is associated with distinct reductions in layer 3 dendritic spine density across primary visual, posterior parietal, and dorsolateral prefrontal cortices.
- Spine size-dependent deficits were regionally specific, affecting small spines in V1 and medium to large spines in PPC and DLPFC.
- Altered fluorescence intensities of F-actin and spinophilin suggest region-dependent changes in synaptic stability and plasticity in SZ.
- Findings suggest that different cortical nodes contributing to visual-spatial working memory are differentially impacted at the synaptic level in SZ.
Study Background
Schizophrenia is a chronic and severe neuropsychiatric disorder characterized by disturbances in cognition, perception, and behavior. Among the cognitive impairments, deficits in visual-spatial working memory are prominent and closely linked to the disease’s functional disability. Visual-spatial working memory depends on the integrity of a distributed cortical network involving the primary visual cortex (V1), posterior parietal cortex (PPC), and dorsolateral prefrontal cortex (DLPFC). The connectivity across these nodes is mediated primarily by excitatory synapses on dendritic spines of pyramidal neurons in layer 3 (L3) of the neocortex.
Abnormalities in dendritic spine density and morphology have long been hypothesized to underlie synaptic pathology in SZ. Dendritic spines are small membranous protrusions that receive excitatory inputs; their density and structure are indicative of synaptic health, plasticity, and stability. Previous studies indicated spine deficits in prefrontal regions in SZ but lacked a comprehensive assessment across multiple cortical areas critical for visual-spatial working memory and differentiation by spine size.
Study Design
This study is a case-control neuropathological investigation involving postmortem brain tissue obtained from 20 individuals with a confirmed diagnosis of schizophrenia and 20 matched unaffected comparison (UC) individuals. Subjects were matched for age, sex (70% male, 30% female in both groups), and other relevant demographic characteristics to minimize confounding.
Brain regions analyzed included the primary visual cortex (V1), posterior parietal cortex (PPC), and dorsolateral prefrontal cortex (DLPFC). Layer 3 pyramidal neurons were isolated for dendritic spine analysis. Spines were fluorescently labeled using phalloidin to stain F-actin, which marks the spine cytoskeleton, and immunolabeling for spinophilin, a protein associated with dendritic spine stability and synaptic function. Confocal microscopy enabled high-resolution imaging and quantitative analyses of spine density, size classes (small, medium, large), and fluorescence intensity.
Key Findings
The primary outcome measures were comparisons of dendritic spine density and size distributions between SZ and UC groups across the specified cortical regions.
1. Dendritic Spine Density Deficits Are Region- and Size-Specific:
– In V1, individuals with SZ had a significant reduction of 18% in the density of small spines (95% CI: -31% to -5%; P = .009).
– In PPC, medium spines were reduced by 16% (95% CI: -28% to -4%; P = .01), and large spines showed a substantial 38% reduction (95% CI: -58% to -17%; P < .001).
– In DLPFC, medium and large spines were also reduced (medium spines: -13%, 95% CI: -21% to -4%; P = .009; large spines: -30%, 95% CI: -50% to -11%; P = .004).
2. Alterations in Spine Structural Markers:
– Phalloidin fluorescence, indicating F-actin content, was decreased in small (-9.5%, P = .04) and medium (-9.8%, P = .04) spines in V1 but paradoxically increased by 9.5% (P = .049) in large spines of DLPFC, suggesting region- and size-specific cytoskeletal remodeling.
– Spinophilin fluorescence intensity was consistently lower across all spine sizes and regions in SZ, ranging from a 13% to 34% decrease (P values .02 to <.001), underscoring a general deficit in synaptic scaffolding proteins.
3. Link to Functional Impairment:
Since dendritic spine size correlates with synaptic properties, with small spines considered more plastic and large/medium spines more stable, these regional patterns suggest that sensory areas (V1) primarily suffer plasticity-related deficits, while association areas (PPC, DLPFC) experience loss in synaptic stability. This pattern mirrors the cognitive deficits in visual-spatial working memory seen in SZ.
Expert Commentary
The findings from Fish et al. add a nuanced understanding of synaptic pathology in schizophrenia, highlighting spatial specificity across the cortical hierarchy and the role of spine size in synaptic vulnerability. This suggests that SZ is not a uniform synaptic pathology but involves differential disruptions that may explain heterogeneous clinical manifestations.
The decreased spinophilin across all regions suggests a shared molecular substrate for synaptic loss, whereas the variable phalloidin changes hint at divergent cytoskeletal responses. The study’s focus on well-matched postmortem samples and advanced imaging techniques adds robustness, though limitations inherent to postmortem analyses, such as possible medication effects and variable agonal states, remain.
Future research integrating these findings with in vivo imaging, electrophysiology, and functional assessments could clarify mechanistic pathways toward developing targeted synaptoprotective interventions.
Conclusion
This comprehensive cortical study elucidates regionally and size-specific dendritic spine deficits in layer 3 pyramidal neurons of individuals with schizophrenia. The differential impact on small versus large spines across visual and association cortices supports a model in which SZ-mediated synaptic pathology disrupts cortical circuits involved in visual-spatial working memory by distinct mechanisms—impaired plasticity in sensory regions and synaptic destabilization in higher-order association areas. These insights provide critical directions for future mechanistic studies and potential therapeutic targets aimed at restoring synaptic integrity and cognitive function in schizophrenia.
Funding and ClinicalTrial.gov
The study was conducted with support from the Allegheny County Office of the Medical Examiner and affiliated academic institutions. No clinical trial registration applies as this is a neuropathological case-control study.
References
Fish KN, Sweet RA, MacDonald ML, Lewis DA. Regional Specificity of Cortical Layer 3 Dendritic Spine Deficits in Schizophrenia. JAMA Psychiatry. 2025 Sep 17:e252221. doi:10.1001/jamapsychiatry.2025.2221. PubMed PMID: 40960807; PMCID: PMC12444653.
Additional relevant literature:
– Glausier JR, Lewis DA. Dendritic spine pathology in schizophrenia. Neuroscience. 2013;251:90-107.
– Glantz LA, Lewis DA. Decreased dendritic spine density on prefrontal cortical pyramidal neurons in schizophrenia. Arch Gen Psychiatry. 2000 Jan;57(1):65-73.
– Penzes P, Cahill ME, Jones KA, et al. Dendritic spine pathology in neuropsychiatric disorders. Nat Neurosci. 2011 Mar;14(3):285-293.