Highlights
- Pre-emptive transjugular intrahepatic portosystemic shunt (p-TIPS) within 72 hours significantly lowers the risk of death or rebleeding compared to glue obliteration plus non-selective β-blockers (NSBB) in patients with cirrhosis and acute fundal variceal bleeding.
- The 1-year probability of survival free from rebleeding was 77% with p-TIPS versus 37% with glue obliteration and NSBB (HR 0.25; 95% CI 0.12–0.51; p<0.0001).
- Rates of hepatic encephalopathy and adverse events were comparable between groups, supporting the safety of early p-TIPS in this high-risk population.
Clinical Background and Disease Burden
Gastric variceal bleeding is a life-threatening complication of portal hypertension in patients with cirrhosis, with acute fundal varices (isolated gastric varices, IGV1) carrying especially high risks of massive hemorrhage and rebleeding. Traditional standard-of-care involves endoscopic glue obliteration (cyanoacrylate injection) for acute control, followed by secondary prophylaxis with repeated glue sessions and NSBB to prevent recurrence. Despite these interventions, outcomes remain suboptimal, with significant rates of recurrent bleeding and mortality within the first year. Thus, there is a substantial unmet need for more effective strategies to improve long-term prognosis in this vulnerable population.
Research Methodology
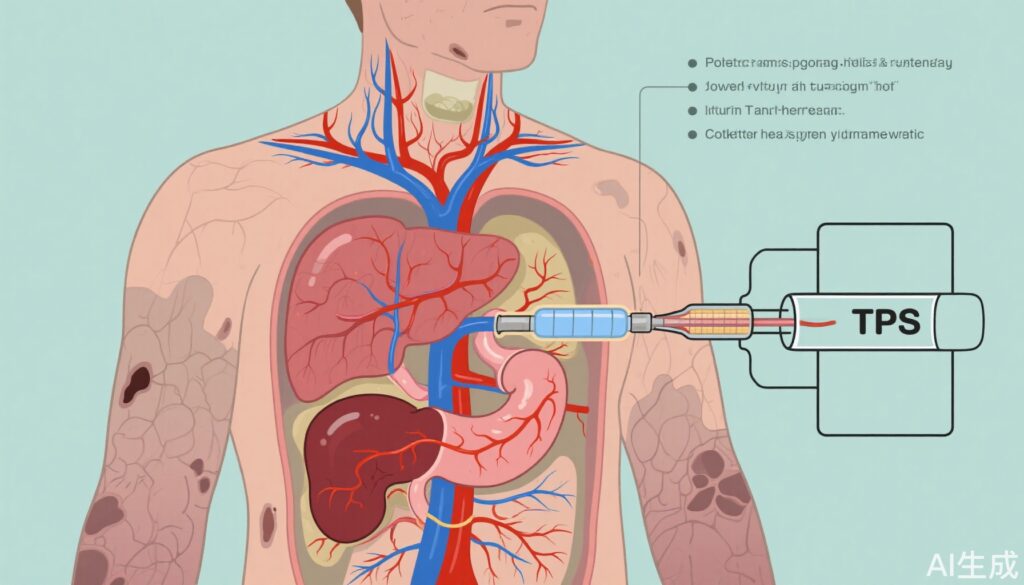
The GAVAPROSEC trial was a multicenter, open-label, randomized controlled trial conducted across 17 tertiary centers in France. The study enrolled adults with cirrhosis and acute fundal variceal bleeding (excluding type 1 gastro-oesophageal varices) who achieved initial hemostasis with endoscopic glue injection and vasoactive therapy, and were clinically stable for at least 12 hours. Participants were randomized (1:1) to either:
- Pre-emptive TIPS (p-TIPS): Placement of a covered TIPS within 72 hours of index bleeding event.
- Standard therapy: Continued on-demand glue obliteration sessions combined with NSBB.
Randomization was stratified by center and performed in blocks. The primary composite endpoint was all-cause mortality or clinically significant rebleeding within 1 year. Secondary outcomes included rates of hepatic encephalopathy, need for rescue TIPS, adverse events, and technical complications such as glue migration. Analyses were conducted on the modified intention-to-treat (mITT) population, defined as all randomized patients excluding those with randomization errors or withdrawal of consent.
Key Findings
Of 292 patients screened, 105 were randomized; after exclusions, 101 were analyzed (mean age 58.2 years, 80% male, 90% with alcohol-related cirrhosis, mean MELD 14.3). Forty-seven patients received p-TIPS, and 54 received glue obliteration and NSBB.
– The 1-year probability of being free from death or rebleeding was 77% (95% CI 62–87) in the p-TIPS group versus 37% (24–50) in the control group (HR 0.25, 95% CI 0.12–0.51; p<0.0001), indicating a 75% relative risk reduction with p-TIPS.
– Rescue TIPS was needed in 37% of control patients, underscoring the inadequacy of standard therapy in many cases.
– Glue migration occurred in 8 patients (3 in p-TIPS, 5 in control), highlighting the procedural risks inherent to glue therapy.
– One case of cardiac decompensation was reported in the p-TIPS group.
– The 1-year cumulative incidence of hepatic encephalopathy was similar between groups (35% in p-TIPS, 32% in control), suggesting no added risk from early TIPS placement.
The trial’s results robustly support the superiority of pre-emptive TIPS in this specific clinical scenario, with strong effect sizes and statistically significant outcomes.
Mechanistic Insights and Biological Plausibility
The rationale for p-TIPS in this context rests on the principle that TIPS effectively decompresses the portal venous system, thereby reducing the pressure driving variceal bleeding. While glue obliteration targets the local varix, it does not address underlying portal hypertension, leaving patients at risk for both rebleeding and new variceal formation. Early intervention with TIPS—before clinical deterioration—may preserve hepatic reserve and reduce morbidity, as evidenced by the lack of increase in hepatic encephalopathy in the GAVAPROSEC trial.
Expert Commentary and Guidelines Perspective
Current international guidelines recommend TIPS as rescue therapy for refractory variceal bleeding, but have been cautious about its pre-emptive use due to concerns regarding encephalopathy and technical risks. The GAVAPROSEC trial, in line with prior evidence from esophageal variceal bleeding studies, now provides high-level data supporting early TIPS in fundal gastric variceal bleeding. As stated by the study authors, early TIPS should be considered first-line therapy for this high-risk group. These findings may prompt guideline revisions and practice changes, particularly in centers with TIPS expertise.
Controversies and Limitations
While the trial is robust in design, several limitations are notable:
– The open-label nature may introduce performance or detection bias, though endpoints were objective.
– The study was conducted exclusively in French tertiary centers with high procedural expertise, potentially limiting generalizability to other settings with less access to TIPS.
– Exclusion of type 1 gastro-oesophageal varices narrows applicability to isolated fundal varices.
– The sample size, though sufficient for primary outcome detection, limits subgroup analysis (e.g., by MELD or etiology).
– Long-term outcomes beyond one year remain to be established.
Conclusion
The GAVAPROSEC trial establishes pre-emptive TIPS as a superior strategy to standard glue obliteration plus NSBB for preventing death or rebleeding in cirrhotic patients with acute fundal variceal bleeding. The intervention is safe, with no excess risk of hepatic encephalopathy, and should be considered first-line therapy in appropriate candidates. Future research is warranted to confirm these findings in broader settings and to refine patient selection criteria.
References
1. Cervoni JP, Weil D, Desmarets M, et al. Pre-emptive TIPS for gastric variceal bleeding in patients with cirrhosis (GAVAPROSEC): an open-label randomised clinical trial. Lancet Gastroenterol Hepatol. 2025 Aug;10(8):726-733. doi: 10.1016/S2468-1253(25)00156-6.
2. Garcia-Tsao G, Abraldes JG, Berzigotti A, et al. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the AASLD. Hepatology. 2017;65(1):310-335.
3. European Association for the Study of the Liver (EASL). EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2022;77(3):807-824.



Can I simply say what a relief to seek out somebody who truly knows what theyre talking about on the internet. You definitely know the right way to deliver a problem to light and make it important. Extra folks must learn this and understand this facet of the story. I cant consider youre no more well-liked since you undoubtedly have the gift.