Study Background and Disease Burden
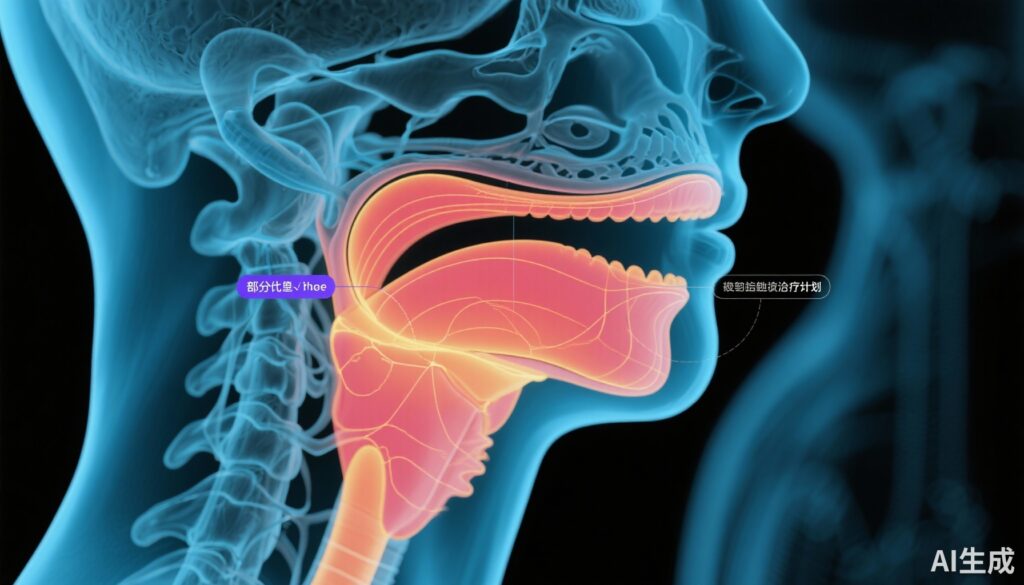
Laryngeal carcinoma represents a significant subset of head and neck squamous cell carcinomas, with early-stage disease (clinical stages T1-2N0M0/Tis) often amenable to curative treatment. The larynx plays a crucial role in phonation, airway protection, and swallowing, making preservation of its function a central therapeutic goal. The current standard treatment for early-stage or in situ laryngeal carcinoma without nodal involvement or distant metastases is whole laryngeal radiotherapy (WLRT). WLRT typically irradiates the entire larynx to manage microscopic disease extension beyond the visibly involved vocal cord. Microsurgical approaches, in contrast, are more focal, removing only the tumor-involved vocal cord with narrow margins. Partial laryngeal radiotherapy (PLRT), which targets only the tumor-involved vocal cord and immediately adjacent tissues, has been proposed as a less toxic alternative but its long-term efficacy and safety profiles have not been well quantified. This gap presents an unmet clinical need to assess whether PLRT can achieve comparable tumor control with reduced toxicities.
Study Design
This article reports a retrospective cohort study conducted at a single tertiary institution, analyzing 233 consecutive patients diagnosed with clinical stage T1-2N0M0 or Tis squamous cell carcinoma of the larynx. These patients underwent intensity-modulated radiotherapy (IMRT), a modern radiation technique allowing conformal dose delivery, between January 2013 and December 2024. Among them, 176 patients received WLRT, and 57 were treated with PLRT. Clinical data were extracted and analyzed between January and February 2025.
Primary endpoints evaluated included long-term locoregional control, laryngectomy-free survival, distant metastasis-free survival, and overall survival. Radiation-associated toxicities both acute and late were documented and graded according to the Common Terminology Criteria for Adverse Events (CTCAE) version 4.0. Patient-reported swallowing-related quality of life was assessed via the MD Anderson Dysphagia Inventory, collected during follow-up visits when feasible.
Key Findings
Median follow-up was notably different between groups: 60 months (interquartile range [IQR], 28-87) for WLRT and 31 months (IQR, 16-64) for PLRT. This difference impacts the comparative strength of long-term outcome assessments.
No statistically or clinically meaningful differences were observed between PLRT and WLRT in key efficacy outcomes at three years:
– Locoregional control was 85.4% in the PLRT group versus 90.8% with WLRT (rate difference -5.4%; 95% CI, -13.5% to 6.9%).
– Laryngectomy-free survival was 93.2% in PLRT versus 94.0% in WLRT (rate difference -0.8%; 95% CI, -9.1% to 7.5%).
– Distant metastasis-free survival was 100% in PLRT and 97.6% in WLRT (rate difference 2.4%; 95% CI, -0.3% to 4.9%).
– Overall survival was similar, 91.4% with PLRT versus 88.9% for WLRT (rate difference 2.5%; 95% CI, -6.8% to 12.8%).
Notably, no cases of contralateral vocal fold failure occurred in the PLRT cohort.
However, stratified analysis revealed a substantial difference in locoregional control for T2 tumors favoring WLRT (85.1%) over PLRT (66.7%), though the confidence interval spanned from -5.8% to 21.3%, indicating uncertainty.
Regarding toxicity, PLRT was associated with significantly lower acute dysphagia incidence (73.7%) than WLRT (92.6%); the absolute difference was 18.9% (95% CI, 6.9% to 30.9%). Swallowing-related quality of life, assessed by median MD Anderson Dysphagia Inventory composite scores, was generally higher in the PLRT group at 3 and 6 months post-treatment (86 vs 77 at 3 months; difference 8 points; 95% CI, 2 to 14; and 96 vs 81 at 6 months; difference 4 points; 95% CI, -2 to 8), although these differences may not reach clinical significance.
Expert Commentary
This study provides important comparative data indicating that partial laryngeal radiotherapy can achieve locoregional control and survival outcomes similar to whole laryngeal RT in early-stage T1 and Tis laryngeal carcinomas, with the potential benefit of reduced acute toxicity and improved early swallowing-related quality of life. The absence of contralateral vocal fold failures in the PLRT group reassures regarding the adequacy of the reduced radiation field in selected patients.
Nevertheless, the shorter median follow-up for the PLRT group limits conclusions about long-term tumor control and late toxicities, which are vital considerations for functional preservation and overall quality of life. The observed lower locoregional control in T2 tumors with PLRT suggests that wider irradiation may be necessary for larger lesions, underscoring the importance of tumor stage in treatment customization.
The retrospective design, lack of randomization, and absence of adjustment for confounding factors such as tumor characteristics, comorbidities, and treatment variations also temper the strength of these findings. Prospective randomized trials are needed to validate PLRT’s efficacy and safety and to define patient selection criteria more precisely.
Biologically, the reduction of irradiation volume in PLRT theoretically spares uninvolved laryngeal structures, preserving mucosal and muscular integrity, which explains the lower incidence of acute dysphagia. This aligns with the growing trend in radiation oncology towards de-escalation strategies aiming to minimize toxicity without compromising tumor control.
Conclusion
Partial laryngeal radiotherapy represents a promising approach for selected patients with early-stage T1 or in situ laryngeal carcinoma, offering comparable 3-year locoregional control and survival rates versus the current standard whole laryngeal radiotherapy. The potential for reduced acute toxicity and improved functional outcomes like swallowing quality of life suggest meaningful clinical benefits. However, based on this retrospective cohort, uncertainty remains due to limited follow-up in the PLRT cohort and possible selection bias.
Until further prospective data emerge, caution is warranted when considering PLRT, especially for T2 lesions, where WLRT might provide better tumor control. Future research should focus on randomized controlled trials with standardization of tumor staging, patient selection, and comprehensive long-term safety and efficacy endpoints.
References
Treechairusame T, Dee EC, Cao C, Wu Y, Yu Y, Gelblum D, Riaz N, McBride SM, Chen L, Shamseddine A, Zakeri K, Tsai CJ, Kang JJ, Ganly I, Cracchiolo JR, Patel S, Cohen MA, Wong RJ, Lee NY. Partial vs Whole Laryngeal Radiotherapy for Clinical Stage T1-2N0M0/Tis Laryngeal Carcinoma. JAMA Otolaryngol Head Neck Surg. 2025 Oct 2:e253214. doi:10.1001/jamaoto.2025.3214. Epub ahead of print. PMID: 41037280; PMCID: PMC12492294.